A Rare Case of Mycosis Fungoides of the Scalp Treated With Electron-Beam Radiation Therapy
Affiliations
- 1 Medicover Cancer Institute, Hyderabad, India
Mycosis fungoides (MF) is the most common cutaneous T-cell lymphoma comprising 44% of cutaneous lymphomas and accounting for less than 1% of non-Hodgkin lymphomas. It is clinically characterized by a focal or diffuse cutaneous patch, plaque, and tumor nodules, and is difficult to diagnose in the early stages because the symptoms and skin biopsy findings are similar to those of other skin conditions such as psoriasis, eczema, and lichenoid dermatoses. Here, we present a case about a patient who presented with a focal nodular skin lesion over the scalp.
Case Summary
A 70-year-old man presented with a cutaneous swelling of 3-month duration over the left side of the scalp. The swelling gradually progressed in size, and no other significant issues were present. The patient was evaluated initially by a dermatologist. Local examination revealed a 3 × 2.5-cm plaque-like keratotic lesion over the scalp on the left side ( Figure 1A ), and the lesion was mobile, nontender, nonpulsatile, and not fixed to the underlying skull bone. No palpable cervical or other regional lymph nodes were found, and no other similar skin lesions elsewhere on the body could be visualized.
Clinical photographs of pretreatment (A) and post-treatment (B) showing complete response.

Laboratory Investigations
Peripheral blood smear showed a normocytic normochromic blood picture with an adequate number of platelets, and white blood cell count was within the normal limits. Mantoux and VDRL (venereal disease research laboratory) tests were negative. Liver function and renal function tests were within the normal limits.
Scalp Lesion Biopsy and Immunohistochemistry
Scalp lesion biopsy and immunohistochemistry (IHC) were CD3 positive in atypical cells, CD4 positive in atypical cells, CD20 negative, CD30 negative, CD8 positive in occasional background cells, and Ki67 8% to 10%. The final impression of morphology and immunohistochemistry correlation was suggestive of folliculotropic mycosis fungoides (MF), plaque stage.
The patient was finally diagnosed with MF, stage 1A (T1N0M0B0), according to the modified TNMB (tumor-node-metastasis-bone marrow) classification, originally adopted by the Mycosis Fungoides Cooperative Study Group. As the skin lesion was localized to a single site, we decided to treat it with radiation therapy. Electron-beam radiation therapy is the modality of choice to treat superficial skin malignant lesions as the tissue-penetrating capacity of electron beam is less compared with photons. Hence, by using electrons, it is possible to treat superficial target volumes without exposing the deep normal tissues to radiation.
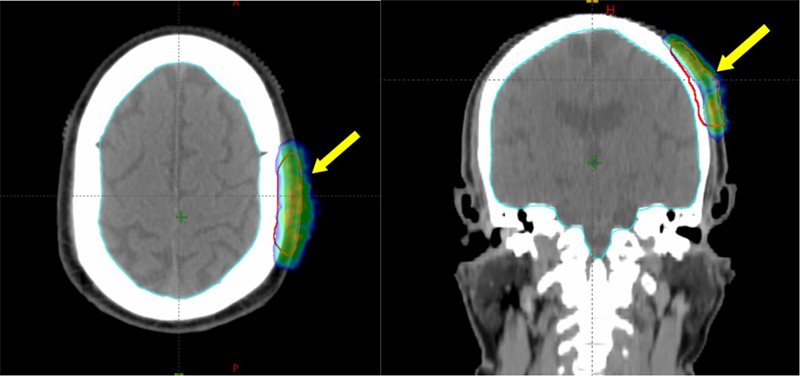
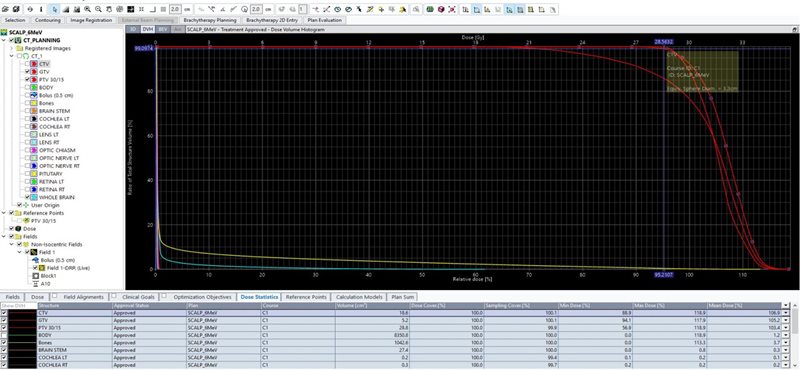
Electron-Beam Treatment Planning Process
Simulation using computed tomography (CT) was performed with the patient immobilized in the supine treatment position using a thermoplastic mask. Target volume was contoured (on the planning CT images), which included the gross scalp lesion visible on clinical examination ( Figure 1A ), planning CT scan, and positron emission tomography/CT (PET/CT) ( Figure 2 ). A 2-cm uniform circumferential clinical target volume (CTV) margin was given to include the possible microscopic extension of the disease in the adjacent surrounding tissue. A 5-mm planning target volume (PTV) margin was given from the CTV to create the final target volume. Treatment planning was done on the Varian Eclipse treatment planning system using a 6-MeV nonisocentric electron beam and a gantry angle of 90° and collimator angle of 0°, with a 5-mm wet cotton bolus covering the PTV. The patient received 30 Gy in 15 fractions, 2 Gy per fraction, 5 days a week over 3 weeks. Figure 3 shows the radiation dose coverage of the target volume. Here, 99% of the gross tumor volume (GTV) and CTV received 95% of the prescribed dose. Also, 94% of the PTV received 85% of the prescribed dose ( Figure 4 ). The patient tolerated the treatment well without any significant side effects. At the end of the treatment, the patient had grade 2 skin reactions (grading based on RTOG [Radiation Therapy Oncology Group] acute radiation morbidity) that subsided over 2 weeks.
Pretreatment positron emission tomography/computed tomography (PET/CT) showing the left scalp lesion (yellow arrow).

Electron-beam treatment plan showing dose coverage (green and blue color wash) of the left parietal scalp lesion. The planning target volume (PTV) is contoured in red.
Dose-volume histogram showing dose coverage details of the treatment plan.
Clinical response assessment was done 3 months after treatment. Clinical examination revealed complete disappearance of the scalp lesion ( Figure 1B ).
Diagnosis
The diagnosis was folliculotropic MF, plaque stage. Differential diagnosis included psoriasis, eczema, and lichenoid dermatoses.
Imaging Findings
Whole-body PET/CT ( Figure 2 ) showed a cutaneous lesion on the left parietal scalp measuring 25 × 7-mm, with a mild 18-fluorodeoxyglucose (FDG) standardized uptake value (SUV)max of 3.5. No other skin lesions were seen, and there was no evidence of any significant lymph nodal or other organ involvement.
Discussion
The cutaneous lymphomas comprise a heterogeneous group of malignancies of both T and B lymphocytes that localize to the skin. The Dutch and Austrian cutaneous lymphoma registries report that more than 70% of all cutaneous lymphomas are of T-cell origin and 22% are of B-cell origin.1, 2 Mycosis fungoides was first reported by Alibert in 1806 as an epidermotropic lymphoma with an indolent evolution characterized by cutaneous lesion in the form of patches, plaques, or skin tumors.3 Both incidence and mortality data demonstrate greater frequency of MF among men than women. The risk also increases with advancing age, and the median age at diagnosis is 55 years.4
One hypothesis regarding the etiology of MF is that it may represent a clonal evolution from chronic antigenic stimulation. Associations with exposure to occupational chemicals or pesticides have also been proposed but not definitely demonstrated in epidemiological studies.5, 6 The association between human T-cell leukemia virus type 1 (HTVL-1) and adult T-cell leukemia/lymphoma is not reflected in the epidemiology of MF, but there are reports of detection of HTVL-1-like viral particles and antibodies to HTVL-1 tax protein in patients with MF.7
The diagnosis of MF is based on clinical and histopathology criteria. The skin manifestations can be in the form of patches, plaques, erythroderma, cutaneous tumors, or ulcers. Early diagnosis can be difficult and may require multiple biopsies obtained from different lesions over time.8 Most commonly, patients present with multifocal involvement of the skin, but localized skin involvement is also common. Extracutaneous involvement may be seen in advanced stages with the involvement of lymph nodes, bone marrow, or, less commonly, other organs. A multidisciplinary team approach involving a hemato-oncologist, dermatologist, radiation oncologist, and pathologist is often optimal for deciding the best management plan. The goals of therapy should be individualized based on the extent of disease.
For diseases confined to the skin lesions with no nodal or other organ involvement, skin-directed therapies such as local radiation, phototherapy, topical corticosteroids, topical retinoids, or topical chemotherapy agents like nitrogen mustard are used and have an excellent chance of cure or long-term control.9 Skin-directed therapies exert their primary effects on the skin by inducing apoptosis of tumor cells and modulation of the immune micro-environment in the skin.
Diffuse involvement of the skin with multiple skin lesions all over the body is usually treated with total skin electron therapy,10 - 13 whereas patients presenting with a solitary focal skin lesion can be treated with focal electron-beam therapy (as presented in this case). Patients with involvement of nodes, bone marrow, or other organs require treatment with systemic chemotherapy.14, 15 The use of supportive care measures to minimize the risk of skin infections and treat pruritus is an important part of disease and symptom control.
Alemtuzumab, a humanized monoclonal antibody that targets the CD52 antigen, has been shown to be active in relapsed or refractory T-cell lymphomas.16
Conclusion
Mycosis fungoides is the most common cutaneous T-cell lymphoma, and is usually not fatal. Most patients with MF exhibit an indolent clinical course with slow progression of the lesions. Most commonly, patients present with multifocal involvement of the skin; localized skin involvement is rarely seen. Localized MF can be safely treated with electron-beam therapy for better local control with minimal treatment-related toxicity.
References
Citation
Prabhakar Mariappan, MD, Mirza Athar Ali, MD, Muntimadugu Babaiah, MD, Gudala Stitha Pragna, DM, Praveen Kumar Singa, MBBS, DNB, Muthulingam Shunmugavel, MSc, Soundarya YSB, MSc, Oviya Manohar, MSc. A Rare Case of Mycosis Fungoides of the Scalp Treated With Electron-Beam Radiation Therapy. Appl Radiat Oncol. 2024;(3):54 - 58.
doi:10.37549/ARO-D-24-00006
September 1, 2024