Emotional-intelligence-centric leadership training for radiation oncologists
Images
SA-CME credits are available for this article here.
Strong direction from a competent leader especially skilled at leading individuals and teams is a well-established expectation in business.1 Moreover, the core set of principles embedded in the emotional intelligence (EI) model are valued for business leaders, with data showing that organizations with successful leaders score high on EI.2,3 Translating these strengths from the business world to medicine, however, is no easy task—especially when a changing medical landscape, with new models of delivery and payment, demand high levels of inter-professional collaboration.4
Traditionally, healthcare leaders have been chosen for strength in their discipline rather than in leadership skills and competencies.5 This is compounded by the fact that few undergraduate/graduate training programs exist in medicine with a longitudinal leadership curriculum, and even fewer with an EI foundation. In the multidisciplinary field of radiation oncology (RO), team-based skills are particularly important; yet current U.S. training programs do not specifically incorporate these elements. Educators have indicated the need for discussion about a leadership curriculum for residents at the national level.6 This is a significant opportunity for the field of RO to set the bar for leadership training in graduate medical education.
Recently, Turner et al reported on a global radiation oncology leader curriculum with 20 leader competency skills defined after an international Delphi consensus study.7 These competencies were housed in 3 broadly defined categories: contributing to the improvement of cancer care delivery in teams and wider health systems, engaging in stewardship of cancer care resources, and demonstrating elements of leadership in practice. In the last category, the development of self-awareness was incorporated by attention to strengths, weaknesses, values, drivers, behaviors, and impact on others. This study demonstrated that developing a global leadership curriculum for radiation oncology is feasible, and is actively being initiated in Canada, Australia and New Zealand. Next year at the annual European Society for Radiotherapy and Oncology (ESTRO) meeting there will even be a new course teaching the principles of leadership for radiation oncologists at the ESTRO educational school.
A resident curriculum in RO for enhancing interpersonal and communication skills as well as professionalism is not well-defined, despite data showing that better doctor-patient communication has been associated with fewer patient complaints8 and medical errors.9 Moreover, while nearly 10 years have passed since The Joint Commission issued its Sentinel Event Alert cautioning that disruptive behaviors of healthcare personnel can compromise patient safety,10,11 many radiation oncology residency programs still struggle with how to incorporate curricula to improve these skills in an already tight agenda.
The value of EI as an essential leadership competency in healthcare has been growing, but data are still mixed.12 For medical students, EI has been associated with building leadership and empathy skills,13,14 and interest is growing in developing a leadership curriculum in undergraduate medical education. While some evidence suggests that leadership training that includes EI can benefit family medicine residents,15,16 others have not shown a benefit to incorporating EI.10 Thus, the question we address in this article is whether an EI-based leadership curriculum has a potential role in the postgraduate medical training of U.S. radiation oncology residents.
Potential EI Model Benefits for RO
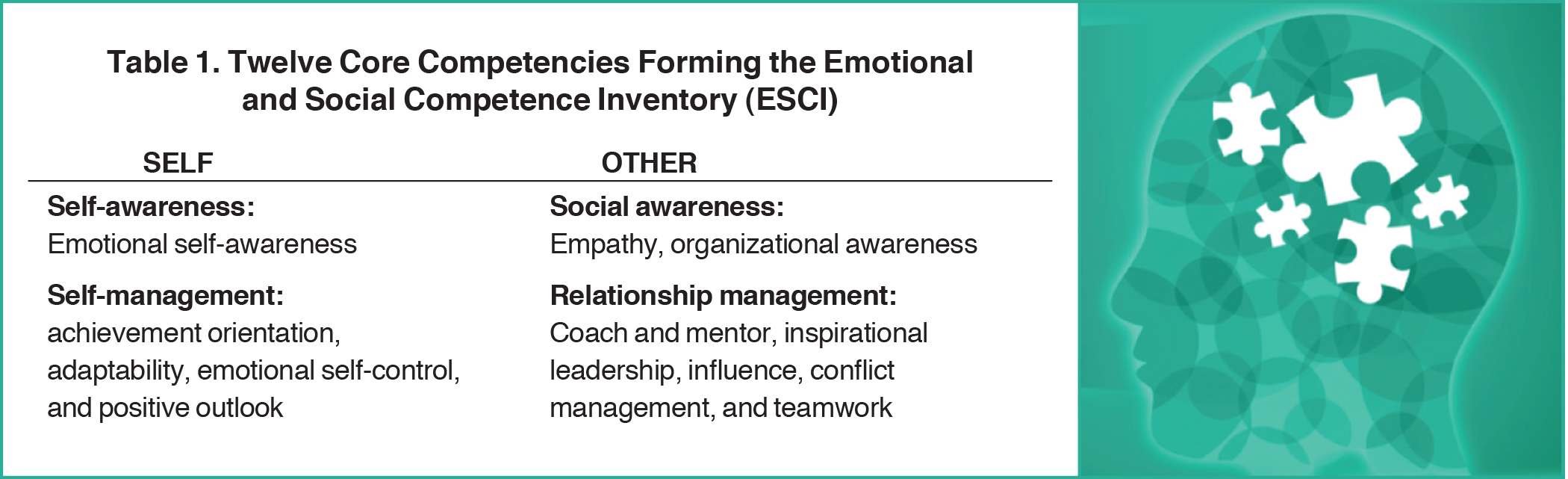
Several models describe and assess EI, with perhaps the best known deriving from the work of Goleman and Boyatzis. In this model, EI consists of 4 quadrants: self-awareness, self-management, social awareness, and relationship management. Although many tools assess EI, one used in business and graduate business education for over 20 years has been the 360-degree survey, the Emotional and Social Competence Inventory (ESCI). The ESCI is comprised of 12 core competencies that form the basis of EI. (See Table 1
.) In the self-awareness quadrant is emotional self-awareness. Within self-management are the competencies of achievement orientation, adaptability, emotional self-control and positive outlook. Social awareness is comprised of empathy and organizational awareness. Finally, 5 competencies form relationship management: conflict management, coach and mentor, influence, inspirational leadership and teamwork.
Goleman has proposed that EI can be learned, as the potential exists for practice-based learning beyond an individual’s intrinsic genetic capabilities.17 This potential resides in the brain’s limbic system, which governs feelings, impulses, and drives that can be “rewired” with practice. This model, thus, has the potential to be “taught” to radiation oncology residents with practice-based learning.
Effectively teaching EI to RO residents could yield multiple downstream benefits. Data at the medical student level have shown poorer specific and overall communication skills as rated by standardized patients in students whose reflections indicate higher emotional withdrawal18 and poor decision-making.19 Since emotion is closely intertwined with the journey of oncology patients and their families, the multiple opportunities for radiation oncology residents to develop empathy during 4 years of training could offer extensive immersion in practice-based learning. At the faculty level, data reported by Pollak et al have shown that when oncologists respond to patients with statements classified as “continuers”
that allow them to express emotion, patients report less anxiety and depression as well as greater satisfaction and adherence to therapy, yet oncologists responded in this manner only 22% of the time.20 Continuer statements allowed the physician to state the patient emotion, empathize with the emotion, praise the strength of the patient, show support, and explore with the patient more of the emotion being expressed. If RO residency training incorporates the first EI quadrant, trainees could not only benefit themselves but also their patients.
In parallel with EI training in self-awareness, developing self-management competencies could yield significant benefits. With accelerating changes in healthcare, increasing feelings of burnout among faculty and resident radiation oncologists have been reported, often attributed to concerns regarding documentation, reimbursement, and patients’ health insurance coverage.21 A study evaluating academic chairs of radiation oncology programs22 noted that major stressors were budget deficits and human resource issues. Additionally, a recent study of academic radiation oncology chairs found that higher EI correlated with low rates of self-reported burnout,23 reinforcing the idea that resident training on self-management, time management, and stress response within the consistent framework of the EI model could help programs nationally decrease burnout within training and prepare residents for resilient postgraduate careers.
As residents gain confidence in recognizing and managing their emotions, the broader context of social awareness may not only lead to the development of empathy with patients, but also with others in the healthcare team. Moreover, the organizational structure of oncology, both in the clinical and research domain, is bathed in a dynamic interplay of multiple disciplines interacting daily. Clinically, residents interact with faculty and staff in the related oncology, surgical and medical subspecialties as well as with colleagues in pathology, radiology, internal medicine, and infectious disease in a variety of settings ranging from tumor boards to inpatient units. During residency, however, trainees are often not exposed to formal training in relationship management.
On the research front, such social awareness and management are no less important, especially given the high-achieving residents who pursue active research projects during training. Recent data show that over 90% of radiation oncology residents perform retrospective research while 20% lead prospective clinical trials, and 50% participate in translational projects.24 These projects immerse residents in teams comprised of other physicians both internal and external to radiation oncology, as well as biostatisticians, basic scientists, computer engineers, mathematical oncologists, and epidemiologists. During such collaborative work, conflicts may arise due to factors such as differences in power dynamics as well as difficulties in team members learning to collaborate, negotiate conflicts, resolve differences, and work effectively in the team environment. However, training in these essential skills is lacking within the traditional radiation oncology resident curriculum.
In the current cancer continuum, the pace of translating discoveries from bench to bedside is exponentially increasing as disruptive technologies continue to evolve with contributions increasingly coming from those in nonbiomedical fields such as computer science and engineering.25 Nationally, there is parallel interest in fostering cross-disciplinary collaboration among health scientists to promote the types of scientific teamwork that can improve population health.26 Recent data support the trend of increasing collaboration in science, with more grant submissions and publications from cross-discipline collaborators vs. within-discipline collaborators.27 In oncology, pairings of basic scientists with clinicians are seen as important foundations to an integrated academic culture to accelerate discovery and innovation.28
With the future inviting more opportunities for collaboration, radiation oncology residents may be in a unique position to serve at the forefront of developing EI-centric leadership competencies. Long term, this has the potential to expand the representation of radiation oncologists in prominent leadership roles at the organizational/institutional level, rather than just the RO departmental level, thus widening the range of the voice of RO as a specialty. Given the smaller class size of residency programs, trainees across all 4 years are in the same lectures, journal clubs, and case conferences. Built into training is the capacity for role modeling of the first-year residents observing the performance of older residents. There is also the “safety” net of a same-discipline cocoon in which trainees can develop skills through engaging role play.
The challenge is how U.S. programs could incorporate such curricula within the confines of an already packed schedule. The structure of the 4-quadrant EI model may potentially provide the best fit in this setting. Such structure could be reinforced with practice-based learning environments in the context of the clinical content taught that day. At the medical student level, simulation labs with standardized patients have fostered clinical skills, and are being used for specifically developing and assessing students’ EI competencies as well. This simulation-based medical education (SBME) has been shown to improve patient safety and, with appropriately structured learning objectives, can focus on individual or team-based activities with attention to communication, collaboration and teamwork, and decision-making.29
With some format modifications, the SBME program could potentially apply to RO residency training in the existing content modules. For example, a tumor board scenario could be designed that would integrate case workup and review as well as journal articles. The faculty lead could assign each resident an appropriate journal article and position to defend. The senior residents could play the roles of medical and surgical oncologists and engage the first year in a conflict scenario. First-year residents would later write a reflection on how they felt when their position was questioned and how they managed their internal response. Senior residents would write a reflection on how their role affected how they spoke to the colleague and what strategies they used to influence the tumor board group to their position. As such, the senior residents would be practicing not only conflict management skills, but also their ability to influence the team. Integrating an EI-centric approach may thus enhance the engagement of the residents and potentially enrich their understanding of the material since they would have to actively assimilate the scientific journal content to best articulate their position to the group. The simulated tumor board group environment could be maximized in the context of case conferences and journal clubs.
The 4-quadrant EI model also has the foundation for integrating it as a coaching tool. Residency programs featuring a coaching approach have traditionally done so with a faculty/resident pairing, with qualitative data suggesting that such coaching dyads during postgraduate training can breed physician leaders who can improve the clinical practices in which they work.30 At the faculty level, peer coaching has been reported to positively impact those who coach as well as those who receive the coaching by contributing to professional development by encouraging reflection time and learning.31 The specifics of the type of dyad model to consider in RO training would need further testing, but given the small numbers of trainees, both the faculty/resident and senior/junior resident may have a role.
An EI-centric approach to leadership training for RO residents may provide a systematic approach to accomplish many of the competencies espoused in the global Delphi consensus study. With respect to improving cancer care delivery in teams and wider health systems, training programs may decide to engage coaching pairs in quality improvement (QI) projects for the department. By working in pairs, the residents would need to seek engagement for the appropriate stakeholders, which would allow them to practice communication skills with staff both inside and outside the department. They would have the opportunity to manage a project, meet deadlines, run meetings, and lead themselves to successful completion. At the end of each year, the projects could be presented orally to the faculty, which would also allow them to practice professionalism skills. To engage residents in cost and resource stewardship, basic training in finance could be taught so projects could have appropriate budgetary metrics to meet. Finally, these yearly projects may provide the opportunity to demonstrate competency in elements of leadership. To complete the project, the resident pairs would need to add other advisors to their team and learn how to influence different stakeholders to accomplish their goal.
Conclusion
The changing healthcare landscape offers increasing opportunities for specialists in radiation oncology to become effective physician leaders in larger organizational settings, spanning both the clinical and research environments. The 4-quadrant EI model has been associated with superior achievement in the business community but has not been validated in RO residency training. A global Delphi consensus study has now defined a leader role curriculum for RO. Further evaluation of an immersive EI-centric leadership training curriculum would be feasible for U.S. residents in radiation oncology.
References
- Offermann LR, Bailey JR, Vasilopoulos NL, Seal C, Sass M. The relative contribution of emotional competence and cognitive ability to individual and team performance. Human Performance. 2004;17:219-243.
- Abraham C. The relationship between emotional intelligence and work attitudes, behavior and outcomes: an examination among senior managers. J Manag Psychol. 2003;18:788-813.
- Higgs M, Aitken P. An exploration of the relationship between emotional intelligence and leadership potential. J Manag Psychol. 2003;18:814-823.
- Bohmer RMJ. Leading cinicians and clinicians leading. N Engl J Med. 2013;368:1468-1470.
- Mintz LJ, Stoller JK. A systematic review of physician leadership and emotional intelligence. J Grad Med Educ. 2014;6:21-31.
- Dinchen J, Ricardo C, Heather S, et al. The need for a leadership curriculum for residents. J Grad Med Educ 2015;7:307-309.
- Turner S, Seel M, Trotter T, et al. Defining a leader role curriculum for radiation oncology: a global Delphi consensus study. Radiother Oncol. 2017;123:331-336.
- Tamblyn R, Abrahamowicz M, Dauphinee D, et al. Physician scores on a national clinical skills examination as predictors of complaints to medical regulatory authorities. JAMA. 2007;298:993-1001.
- Singh H, Thomas EJ, Petersen LA, Studdert DM. Medical errors involving trainees: a study of closed malpractice claims from 5 insurers. Arch Intern Med. 2007;167:2030-2036.
- Webb AR, Young RA, Baumer JG. Emotional intelligence and the ACGME competencies. J Grad Med Educ. 2010;2:508-512.
- Rosenstein AH, O’Daniel M. A survey of the impact of disruptive behavior and communication defects on patient safety. Jt Comm J Qual Patient Saf. 2008:34(8)464-471.
- Lobas JG. Leadership in academic medicine: capabilities and conditions for organizational success. Am J Med. 2006;119:617-21.
- Hojat M, Vergare MJ, Maxwell K, et al. The devil is in the third year: a longitudinal study of erosion of empathy in medical school. Acad Med. 2009;84:1182-1191.
- Rosenthal S, Howard B, Schlussel YR, et al. Humanism at heart: preserving empathy in third-year medical students. Acad Med. 2011;86:50-358.
- O’Brien-Gonzales A, Chessman AW, Sheets KJ. Family medicine clerkship curriculum: competencies and resources. Fam Med. 2007;39:43-46.
- Kuo AK, Thyne SM, Chen HC, West DC, Kamei RK. An innovative residency program designed to develop leaders to improve the health of children. Acad Med. 2010;85:1603-1608.
- Goleman D, Boyatzis R. Emotional intelligence has 12 elements. Which do you need to work on? Harv Bus Rev. February 2017.
- Shapiro J, Lie D. A comparison of medical students’ written expressions of emotion and coping and standardized patients’ ratings of student professionalism and communication skills. Med Teach. 2004;26:733-735.
- Damasio AR. Decartes’ Error: Emotion, Reason, and the Human Brain, New York: Putnam Publishing; 1994.
- Pollak KI, Arnold RM, Jeffreys AS, et al. Oncologist communication about emotion during visits with patients with advanced cancer. J Clin Oncol. 2007;25:5748-5752.
- Pohar S, Fung CY, Hopkins S, et al. American Society for Radiation Oncology (ASTRO) 2012 Workforce Study: the radiation oncologists’ and residents’ perspectives. Int J Radiat Oncol Biol Phys. 2013;87:1135-1140.
- Kusano AS, Thomas CR, Jr., Bonner JA, et al. Burnout in United States academic chairs of radiation oncology programs. Int J Radiat Oncol Biol Phys. 2014;88:363-368.
- Holliday EB, Bonner JA, Formenti SC, et al. Emotional intelligence and burnout in academic radiation oncology chairs. J Healthc Manag. 2017;62:302-313.
- Nabavizadeh N, Burt LM, Mancini BR, et al. Results of the 2013-2015 Association of Residents in Radiation Oncology Survey of Chief Residents in the United States. Int J Radiat Oncol Biol Phys. 2016;94:228-234.
- Welch DR, Antalis TM, Burnstein K, et al. Essential components of cancer education. Cancer Res. 2015;75:5202-5205.
- Hall KL, Stokols D, Moser RP, et al. The collaboration readiness of transdisciplinary research teams and centers findings from the National Cancer Institute’s TREC Year-One evaluation study. Am J Prev Med. 2008;35:S161-172.
- Luke DA, Carothers BJ, Dhand A, et al. Breaking down silos: mapping growth of cross-disciplinary collaboration in a translational science initiative. Clin Transl Sci. 2015;8:143-149.
- Feldman AM. Bench-to-Bedside; Clinical and Translational Research; Personalized Medicine; Precision Medicine-What’s in a Name? Clin Transl Sci. 2015;8:171-173.
- Sorensen JL, Ostergaard D, LeBlanc V, et al. Design of simulation-based medical education and advantages and disadvantages of in situ simulation versus off-site simulation. BMC Med Ed. 2017;17:20.
- Homa K, Regan-Smith M, Foster T, et al. Coaching physicians in training to lead improvement in clinical microsystems: a qualitative study on the role of the clinical coach. Int J Clin Leadersh. 2008;16:37-48.
- Sekerka LE, Chao J. Peer coaching as a technique to foster professional development in clinical ambulatory settings. J Contin Educ Health Prof. 2003;23:30-37.
Citation
SE H, J Q, J F, TJ D, NA S, LB H. Emotional-intelligence-centric leadership training for radiation oncologists. Appl Radiat Oncol. 2017;(4):8-12.
December 14, 2017