MRI Links Breast Tissue Features With Future Second Breast Cancer Risk
 A study published in Radiology has linked breast tissue features apparent on MRI with future second breast cancer risk in women with a personal history of breast cancer.
A study published in Radiology has linked breast tissue features apparent on MRI with future second breast cancer risk in women with a personal history of breast cancer.
Breast cancer survivors with dense breasts face an even greater risk of a second cancer. Breast tissue is mostly fatty, with areas of fibrous connective tissue and glandular tissue known collectively as fibroglandular tissue. Women with dense breasts have a greater proportion of fibroglandular tissue and less fatty tissue. This can obscure lesions on mammography and is an independent risk factor for breast cancer.
Breast MRI has become the preferred method for imaging women with personal history of breast cancer. Previous studies have shown that breast MRI has a higher cancer detection rate than mammography.
“Postoperative surveillance breast MRI is increasingly being performed according to the American College of Radiology’s annual recommendation for women with dense breasts or those diagnosed with breast cancer before age 50,” said study lead author Su Hyun Lee, MD, PhD, from the Department of Radiology at Seoul National University Hospital in Seoul, Korea.
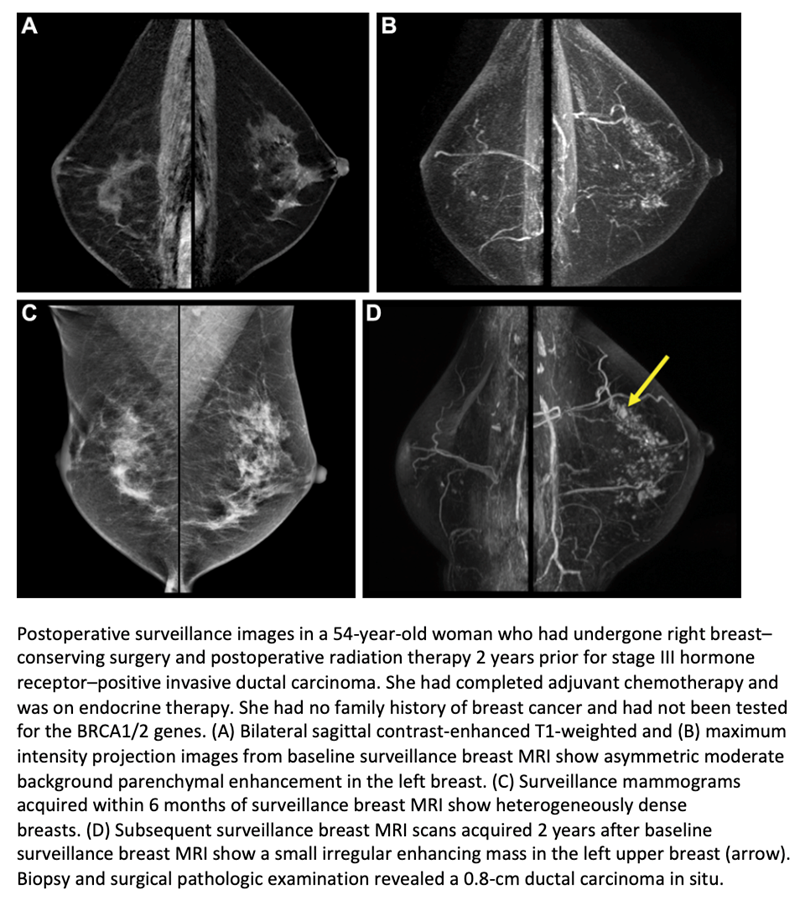
Dr Lee and colleagues studied the link between second cancer risk and background parenchymal enhancement (BPE) at surveillance breast MRI. BPE refers to the brightening, or enhancement, of background tissue on MRI after administration of a contrast agent. The degree of BPE can vary between and within women. It is thought to be related to changes in the blood supply and permeability of breast tissue, which is affected by hormonal status. Breast cancer treatment in the form of radiation therapy, chemotherapy or endocrine therapy can also alter the BPE in the treated breast.
BPE on contrast-enhanced breast MRI is a known risk factor for breast cancer. Less is known about the links between BPE at surveillance breast MRI and the risk of second breast cancer.
Of the 2,668 women in the study, 109 developed a second breast cancer at a median follow-up of 5.8 years. Mild, moderate, or marked BPE at surveillance breast MRI was independently associated with an increased risk of future second breast cancer compared to minimal BPE.
“The results suggest that BPE at postoperative surveillance breast MRI may indicate the response to breast cancer treatment and may be a predictor of the modified risk of second breast cancer after treatment in women with a personal history of breast cancer,” Dr Lee said.
The study findings point to a role for BPE measurements in refining screening pathways for women with prior breast cancer, Dr Lee said.
“Our study results may help to stratify the risk of second breast cancer in women with a personal history of breast cancer and to establish personalized imaging surveillance strategies in terms of imaging modality and monitoring interval selection,” she said. “For example, women with minimal BPE at surveillance breast MRI may no longer need to undergo contrast-enhanced breast MRI every year if other risk factors are absent.”
Those other risk factors include younger age at diagnosis, the presence of genetic mutations linked to breast cancer and hormone receptor expression in the initial breast cancer.
Areas for future study include the link between BPE changes at screening or preoperative breast MRI and at postoperative surveillance breast MRI and the development of second breast cancer.
In the future, Dr Lee expects that risk models will use mammography, ultrasound and MRI together. This approach, she said, will lead to more tailored surveillance strategies for women with a history of breast cancer.