MRI may Help in Fight Against Mesothelioma
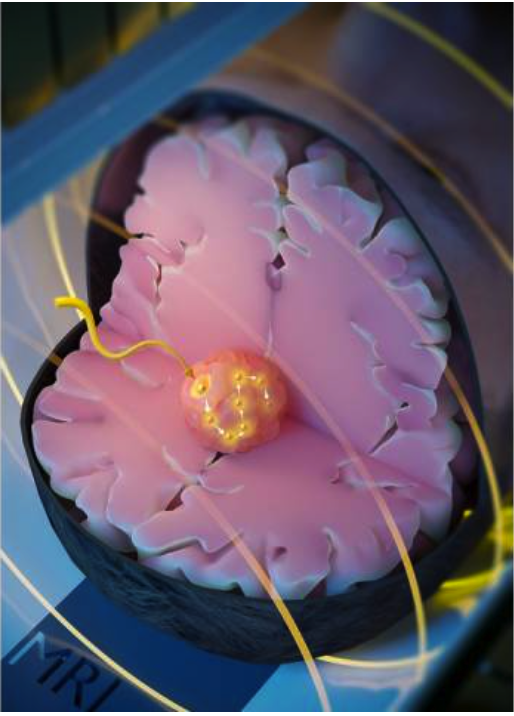 The use of MRI may be provide benefit to those with the rare, asbestos-related form of cancer, mesothelioma. Scientists from the Centre for Advanced Biomedical Imaging at the University College of London (UCL) recently developed a novel cancer therapy that uses an MRI scanner to guide a magnetic seed through the brain to heat and destroy tumors.
The use of MRI may be provide benefit to those with the rare, asbestos-related form of cancer, mesothelioma. Scientists from the Centre for Advanced Biomedical Imaging at the University College of London (UCL) recently developed a novel cancer therapy that uses an MRI scanner to guide a magnetic seed through the brain to heat and destroy tumors.
The therapy, demonstrated in mice, is called “minimally invasive image-guided ablation” or MINIMA and comprises a ferromagnetic thermoseed navigated to a tumor using magnetic propulsion gradients generated by an MRI scanner, before being remotely heated to kill nearby cancer cells.
Researchers say the findings, published in Advanced Science, establish ‘proof-of-concept’ for precise and effective treatment of hard-to-reach glioblastoma, along with other cancers such as prostate, that could benefit from less invasive therapies.
Senior author, Professor Mark Lythgoe, UCL Centre for Advanced Biomedical Imaging, said, “MINIMA is a new MRI-guided therapy that has the potential to avoid traditional side effects by precisely treating the tumor without harming healthy tissues. Because the heating seed is magnetic, the magnetic fields in the MRI scanner can be used to remotely steer the seed through tissue to the tumor. Once at the tumor, the seed can then be heated, destroying the cancer cells, while causing limited damage to surrounding healthy tissues.”
In the study, the UCL team demonstrate the three key components of MINIMA to a high level of accuracy: precise seed imaging; navigation through brain tissue using a tailored MRI system, tracked to within 0.3 mm accuracy; and eradicating the tumor by heating it in a mouse model.
Ferromagnetic thermoseeds are spherical in shape, 2 mm in size and are made of a metal alloy; they are implanted superficially into tissue before being navigated to the cancer.
Lead author, Rebecca Baker, a PhD student at UCL, said, “Using an MRI scanner to deliver a therapy in this way allows the therapeutic seed and the tumor to be imaged throughout the procedure, ensuring the treatment is delivered with precision and without having to perform open surgery. This could be beneficial to patients by reducing recovery times and minimizing the chance of side effects.”
MRI scanners are readily available in hospitals around the world and are pivotal in the diagnosis of diseases such as cancer. The work at UCL shows that MINIMA has the potential to elevate an MRI scanner from a diagnostic device to a therapeutic platform.
Professor Lythgoe added, “We are now able to image and navigate a thermoseed in real-time through the brain using an MRI scanner. As MRI is already used to detect the boundaries of cancers, the seed can be moved precisely to ensure it does not stray into surrounding healthy tissue. As the seed is guided through the tissue it can be heated to destroy the cancer. This combines therapy and diagnosis into a single device, creating a completely new class of imaging therapy.”
Co-author Dr. Lewis Thorne, a consultant neurosurgeon at the National Hospital for Neurology and Neurosurgery, said, “I treat patients with the most common form of brain cancer, glioblastoma. Following surgery, the average survival time is 12-18 months. MINIMA can successfully destroy cancer in a mouse and has the potential to extend survival and limit damage to adjacent brain tissues in patients.”
Professor Mark Emberton, UCL Division of Surgery and Interventional Science, lead cancer clinician in the study, said, “Improving the precision of our cancer treatments is arguably one of the greatest unmet needs we have today.
“One in eight men will be diagnosed with prostate cancer. While treatments such as radiotherapy and surgery can be effective, they often cause unwanted and debilitating side effects such as incontinence and impotence. MINIMA may allow us to precisely target and destroy prostate tumor tissue, reducing harm to normal cells.”
“In the longer term,” Professor Lythgoe added, “we will change the shape of the seed to act as a tiny cutting scalpel that could be guided through tissue, which would allow surgeons to perform remotely controlled operations, revolutionizing non-invasive surgery.”