Mwanza, Tanzania: Challenges and change in RT delivery during global health residency
Images




As a global health resident at Duke University and an Association of Residents in Radiation Oncology (ARRO) Global Health Scholar, I was fortunate to spend 4 months at Bugando Medical Centre (BMC) in Mwanza, Tanzania, during my radiation oncology residency. My initial visits to the oncology clinic at BMC predated their ability to treat patients with radiation therapy (RT), but in my final visit, RT became operational. It was highly gratifying to see patients in need receiving appropriate treatment.
The United Republic of Tanzania is a low-income country of approximately 49 million people in eastern sub-Saharan Africa and an estimated 46% of Tanzanians live below the poverty line of $1.90 per day. BMC is a tertiary care referral hospital in Mwanza, Tanzania, the largest city in the Lake Zone of northwestern Tanzania (Figure 1).
BMC is the only hospital in the Lake Zone with fellowship-trained oncologists for adult oncology, pediatric hematology/oncology and radiation oncology. The Tanzanian government supported BMC’s creation of a dedicated oncology clinic in 2012 (Figure 2).
RT Services and Staff
RT services at BMC were planned to commence in 2014; however, implementing RT was delayed by technical and human capacity limitations. The BMC RT center contains 4 vaults with sufficient shielding for megavoltage teletherapy, 1 vault for orthovoltage therapy, 2 simulator rooms, and 1 brachytherapy suite suitable for high-dose rate brachytherapy. The BMC RT department began treating patients in August 2017. Current equipment includes a single Bhabhatron-II cobalt-60 teletherapy unit (Panacea Medical Technologies, Bangalore, India) and an IMAGIN simulator (Panacea Medical Technologies, Bangalore, India) capable of fluoroscopy, digital X-ray generation, and cone-beam computed tomography (CT) image acquisition. Two multi-energy linear accelerators have been donated but are currently nonoperational, primarily due to the high cost of a service contract (Figure 3).
Current staff at BMC includes 1 radiation oncologist, 1 medical physicist, 2 radiation therapists, and 1 nurse. My clinical experience focused on the oncologic care of cancer patients in both the outpatient and inpatient settings. Before BMC could offer RT services, a typical clinical encounter included a history and physical examination, recommending additional testing for diagnosis or staging, and/or a prescription for treatment. Staging studies for many malignancies were difficult and expensive to acquire, particularly cross-sectional imaging, so cheaper tests such as x-rays and ultrasounds were often used in lieu of computed tomography (CT). Magnetic resonance imaging (MRI) was not available in that region of Tanzania. In addition to my outpatient responsibilities, I rounded with the clinical team at least twice a week. I rounded with the adult oncology and pediatric oncology services and saw a wide range of patients with cancers.
Cancer Cases
Typically, cancer cases in both the outpatient and inpatient setting were locally advanced and/or metastatic. The reasons for this outcome appear to be multifactorial, but clinical suspicion for cancer at the primary care level appears to be low. As mentioned above, accessing and paying for a workup is out of reach for most Tanzanians. On a cultural and societal level, there is a significant stigma associated with a cancer diagnosis. I suspect many patients choose not to pay for a workup because they believe cancer is a uniformly fatal diagnosis and paying for a staging workup and treatment is a futile endeavor.
BMC treated its first patient with RT in the fall of 2017 (Figure 4).
She was a grandmother in her mid-50s who had experienced intermittent vaginal bleeding for several months. She was told by the medical practitioners at her local medical facility that this was of no serious concern. Her bleeding worsened and she then developed pelvic pressure and pain. She was eventually seen by a gynecologist, who performed a vaginal exam and identified a large mass arising from the cervix. A biopsy confirmed squamous cell carcinoma. She had clinical evidence of pelvic sidewall involvement with no evidence of distant metastases by chest x-ray and abdominal ultrasound. She completed a course of definitive external-beam radiation therapy utilizing AP/PA (anteroposterior/posterioranterior) fields to 45 Gy with concurrent cisplatin. A brachytherapy boost would only be available at Ocean Road Cancer Institute in Dar es Salaam, the most populous city in Tanzania more than 1,100 km from Mwanza. She was referred there, although I do not know whether she was able to afford the trip.
Research Efforts
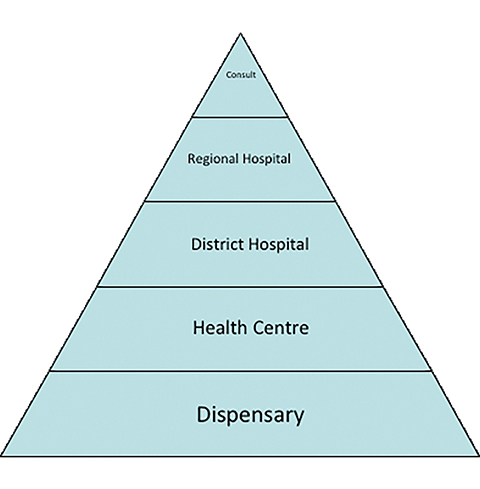
In addition to my clinical rotation, I performed some basic epidemiologic research utilizing a hospital-based cancer registry. I validated, assessed, and utilized the BMC cancer registry to guide RT services planning for BMC. I compared the number of cases at BMC to epidemiologic benchmarks used internationally based on the expected number of cases for the Lake Zone population. Because the dataset I used is a hospital-based registry and not population-based, a thorough understanding of the local healthcare delivery environment is important to provide context. BMC is 1 of 3 tertiary consultant hospitals in Tanzania and the only cancer center in the Lake Zone Region of Tanzania. While BMC saw roughly 12% of the expected cancer patients within the Lake Zone region, it is unknown how many are seen in local health care facilities. Entry into the health care system is often initiated at the local dispensary level or health centers, which is attended by medical assistants and nurses, and typically provides preventive services (eg, vaccines, maternal-child health) with limited laboratory or diagnostic testing. There is typically 1 for every 50,000 people. These refer to District Hospitals, then Regional Hospitals, and finally 1 of the 3 consultant hospitals where diagnostic capacity for cancer exists (Figure 5).
I validated the cancer registry data by comparing it to the patient charts and determined that the concordance was acceptably high. I then determined the expected RT utilization rate to be approximately 56%, significantly higher than most developed countries and likely due to the high rate of locally advanced cervical cancer. Current RT capacity at BMC, unfortunately, falls far short of the clinical need. Human resources, teletherapy, and brachytherapy are required to meet the RT need for the Lake Zone.
Conclusion
In conclusion, my experience at BMC was a highlight of my residency training. It was informative and compelling. My current practice at UPMC Hillman Cancer Center includes consulting on challenging cancer cases with UPMC’s many international collaborative efforts. As radiation therapy is an essential component of cancer care, expanding RT access is a clinical and moral imperative.
Citation
Olson AC. Mwanza, Tanzania: Challenges and change in RT delivery during global health residency. Appl Rad Oncol. 2019;(2):41-43.
July 11, 2019
