New Immuno-Oncology Approach for Most Common Lung Cancer Identified
 A preclinical study from researchers at the Icahn School of Medicine at Mount Sinai has identified a potential new therapeutic approach to treating the most common form of lung cancer. The strategy, described in an online issue of Nature Immunology, involves inhibiting the immune-system molecule TREM2 while enhancing natural killer cells (the so-called protectors of the immune system).
A preclinical study from researchers at the Icahn School of Medicine at Mount Sinai has identified a potential new therapeutic approach to treating the most common form of lung cancer. The strategy, described in an online issue of Nature Immunology, involves inhibiting the immune-system molecule TREM2 while enhancing natural killer cells (the so-called protectors of the immune system).
“Our study reveals that macrophages expressing the molecule TREM2 drive the depletion and dysfunction of effector immune cells called natural killer cells, known to play a key role in the elimination of cancer cells, providing a strong rationale for the clinical development of combination therapies that concurrently block TREM2 and boost natural killer cells,” said first author Matthew Park, an MD/PhD candidate in the lab of Miriam Merad, MD, PhD, senior author of the study. Dr Merad is Director of the Precision Immunology Institute and Director of the Human Immune Monitoring Center at Icahn Mount Sinai.
Previous research has shown that many tumors from patients with non-small-cell lung cancer—the most common type, accounting for 85 percent of all lung cancers—and other cancers are deprived of these natural killer cells, which ordinarily have an innate ability to destroy cancer cells. In recent years, experts have made significant progress in understanding how tumors evade these cells when they are present. However, it remains unclear why these cells are absent from the tumors in the first place, according to the investigators.
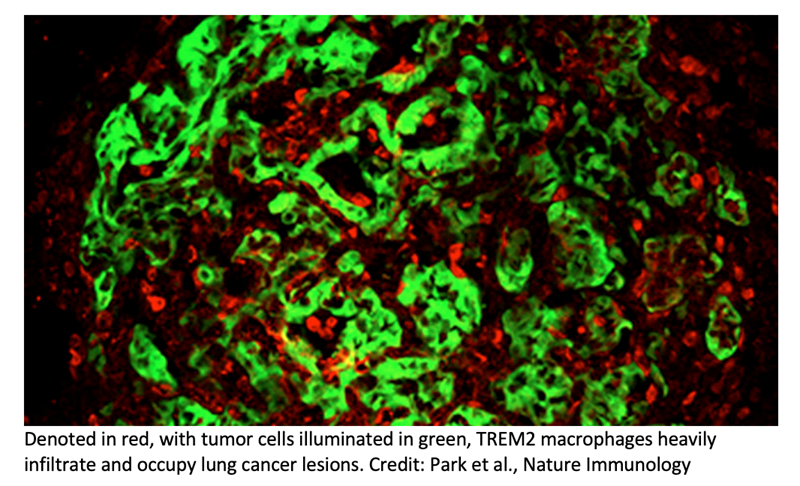
In the current study, macrophages, another type of immune cell, were identified as the culprit. During tumor progression, the researchers found that bone marrow macrophages act to suppress the recruitment and activation of natural killer cells.
To learn why these macrophages have this effect, the research team performed sequencing to determine what genes may be at play, implicating the TREM2 molecule as highly expressed.
Finally, they discovered that inhibiting TREM2 activity using either mice with this mutation or blocking it from binding with an antibody significantly reduced lung tumor growth in mice.
“We identified a novel axis of immunity, whereby TREM2-expressing macrophages regulate the recruitment and activity of natural killer cells during lung tumor progression, and showed preclinical evidence for a new therapeutic strategy that combines TREM2 blockade and natural killer cell activation using an antibody developed by Dr. Ferrari de Andrade,” said Dr. Merad.
Lucas Ferrari de Andrade, PhD, a co-author of the paper, is Assistant Professor of Oncological Sciences at Icahn Mount Sinai. He is a member of the Precision Immunology Institute and the Tisch Cancer Center.
The researchers caution that although TREM2-expressing bone marrow-derived macrophages have been implicated in other tumor types, recent studies suggest TREM2 inhibition is not universally therapeutic. The Icahn Mount Sinai researchers intend to elucidate the applicability of this axis of immunity in other cancers.