Industry NewsBreast CancerGynecologic CancerLung/Thoracic CancerProstate CancerSurvivorship/Late Effects
NIH Finds Prevention and Screening are Major Contributors to Saving Lives in Five Cancer Types
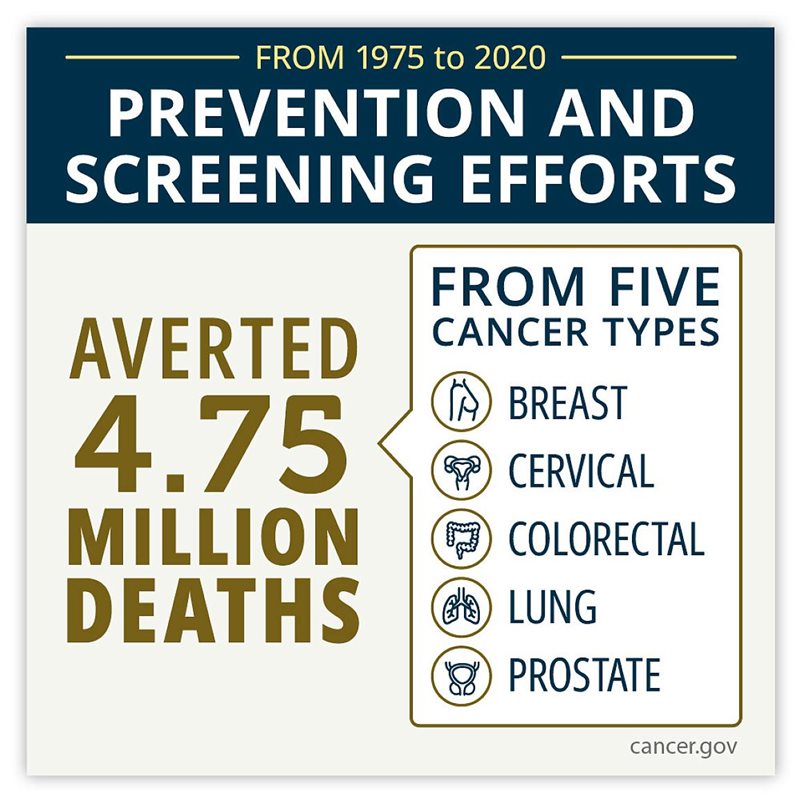 Improvements in cancer prevention and screening have averted more deaths from five cancer types combined over the past 45 years than treatment advances, according to a modeling study led by researchers at the National Institutes of Health (NIH). The study, published in JAMA Oncology, looked at deaths from breast, cervical, colorectal, lung, and prostate cancer that were averted by the combination of prevention, screening, and treatment advances. The researchers focused on these five cancers because they are among the most common causes of cancer deaths and strategies exist for their prevention, early detection, and/or treatment. In recent years, these five cancers have made up nearly half of all new cancer diagnoses and deaths.
Improvements in cancer prevention and screening have averted more deaths from five cancer types combined over the past 45 years than treatment advances, according to a modeling study led by researchers at the National Institutes of Health (NIH). The study, published in JAMA Oncology, looked at deaths from breast, cervical, colorectal, lung, and prostate cancer that were averted by the combination of prevention, screening, and treatment advances. The researchers focused on these five cancers because they are among the most common causes of cancer deaths and strategies exist for their prevention, early detection, and/or treatment. In recent years, these five cancers have made up nearly half of all new cancer diagnoses and deaths.
"Although many people may believe that treatment advances are the major driver of reductions in mortality from these five cancers combined, the surprise here is how much prevention and screening contribute to reductions in mortality," said co-lead investigator Katrina A. B. Goddard, PhD, director of NCI’s Division of Cancer Control and Population Sciences. “Eight out of 10 deaths from these five cancers that were averted over the past 45 years were due to advances in prevention and screening.”
A single prevention intervention, smoking cessation, contributed the lion’s share of the deaths averted: 3.45 million from lung cancer alone. When considering each cancer site individually, prevention and screening accounted for most deaths averted for cervical, colorectal, lung, and prostate cancer, whereas treatment advances accounted for most deaths averted from breast cancer.
“To reduce cancer death rates, it's critical that we combine effective strategies in prevention and screening with advances in treatment,” said W. Kimryn Rathmell, MD, PhD, director of NCI. “This study will help us understand which strategies have been most effective in reducing cancer deaths so that we can continue building on this momentum and hopefully increase the use of these strategies across the United States.”
The researchers used statistical models and cancer mortality data to estimate the relative contributions of prevention, screening, and treatment advances to deaths averted from breast, cervical, colorectal, lung, and prostate cancers between 1975 and 2020.
In total, the modeling showed, 5.94 million deaths were averted from these five cancers between 1975 and 2020. Of these, prevention and screening interventions accounted for 4.75 million, or 80%, of the averted deaths.
The individual contributions of prevention, screening, and treatment varied by cancer site:
- In breast cancer, 1 million deaths (out of 2.71 million that would have occurred in the absence of all interventions) were averted from 1975 to 2020, with treatment advances contributing to three-quarters of the deaths averted and mammography screening contributing to the rest.
- In lung cancer, prevention through tobacco control efforts accounted for 98% of the 3.45 million deaths averted (out of 9.2 million), and treatment advances accounted for the rest.
- In cervical cancer, the 160,000 deaths averted (out of 370,000) were entirely through cervical cancer screening (i.e., Pap and HPV, or human papillomavirus, testing) and removal of precancerous lesions.
- In colorectal cancer, of the 940,000 deaths averted (out of 3.45 million), 79% were due to screening and removal of precancerous polyps, with treatment advances accounting for the remaining 21%.
- In prostate cancer, of the 360,000 deaths averted (out of 1.01 million), screening via PSA testing contributed 56% and treatment advances contributed 44%.
“These findings suggest that we need to continue to have strong strategies and approaches in all of these areas,” Dr. Goddard noted. “It's not just treatment advances alone, or prevention and screening alone, that is helping us to reduce cancer mortality.”
The authors pointed out that more recent prevention and screening strategies, such as HPV vaccination and lung cancer screening, were not in wide use during the study period and could further reduce cancer death rates. Other opportunities for reducing cancer deaths include making screening more accessible, such as with HPV tests that allow for self-collection, and developing new treatments.
The authors acknowledged that the five cancer sites included in the study account for less than half of all cancer deaths and that the findings for these cancers may not necessarily apply to other cancers, especially those for which there are not effective prevention, screening, or treatment interventions.
“We need to optimize the uptake and use of prevention and screening for these five cancers so that all Americans can benefit, especially underserved populations, as well as develop novel prevention and screening strategies to avert deaths due to other, very lethal cancers, such as those of the pancreas and ovary,” said co-lead investigator Philip E. Castle, PhD, MPH, director of NCI’s Division of Cancer Prevention.
In addition, the authors noted that the findings are based on population averages in the United States and may not be generalizable to specific population groups. The study also did not consider the potential harms of interventions, such as false-positive results and overdiagnosis during screening, nor did it measure other outcomes, such as quality of life.