Oncology EMRs: More than a patient record
Images

In health care, an electronic medical record (EMR) is often viewed as a digital version of a paper-based patient record. It tracks data over time; identifies patients due for screenings or other preventive examinations; and can help clinicians compare patients against certain measures or groups, such as vaccinations or medical tests.
Yet in oncology, the EMR is more than a repository of patient information or data source for analytics. It documents activities, optimizes treatments, simplifies management of complex therapies, and helps ensure safe patient care.
“The oncology EMR is the window to the soul of the department,” says Marc D. Posner, MD, medical director, Center for Advanced Radiation Medicine, Northwestern Lake Forest Hospital, Lake Forest, Illinois. “It is a solution that we interact with every day.”
In fact, Dr. Posner says he and his staff interact with the EMR more than the treatment delivery machine or linear accelerator. A key reason: The oncology EMR helps perform three distinct functions in his practice—record and verify, maintain patient records and films, and treatment planning.
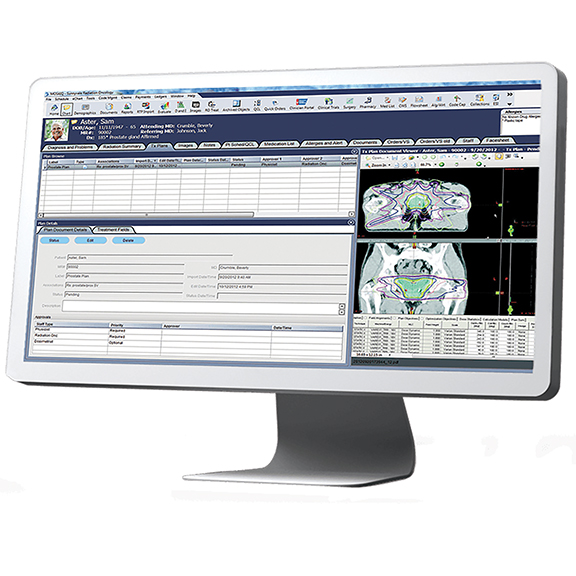
Because of this, the most important feature of an oncology EMR is the integration to other systems, Dr. Posner says. Dr. Posner’s practice has been using MOSAIQ (Elekta, Stockholm, Sweden) for more than 10 years, and he has experienced the ongoing integration of modules, such as treatment planning, into MOSAIQ.
“Having the treatment plans available in the oncology EMR for the physician to review and approve is huge,” he says. “Since I don’t have treatment planning software on my computer, previously I would go into the physics department and interrupt what they were doing in order for me to review and approve. Now, our physicist electronically pushes the plan to me and I can review it right in my office on my desktop computer.”
This workflow efficiency in reviewing and approving plans saves time for Dr. Posner and his physicist, further benefitting patient care. “Right now, we are operating at a very efficient pace with an incredibly fast turn-around-time on plans and quality assurance—from simulation to treatment,” he adds.
“There’s a second advantage to having the plan in the EMR,” says Dr. Posner. “If that patient needs further treatments then we need to know [details regarding] what they had the first time.” Or, for example, if a dentist needs dose information on a patient treated for oral cancer, he can pull up the information, export it to a PDF and email it. “I can answer these questions immediately—even in 15 seconds—and that’s so important for patient care.”
Transitioning to Value-based Care
The shift in the U.S. health care system to a value-based care environment will also require changes in IT systems and software, explains Sukhveer Singh, vice president of Oncology Continuum Solutions, Varian Medical Systems, Palo Alto, California.
“The next transformation is what we do with the data to make better care decisions, promote rapid learning, and advance patient outcomes,” Singh says. “Big data has meaning in oncology—the information in our systems is a collective digital experience. How we use that experience to coordinate care is extremely important in oncology.”
To achieve big data analytics, system integration needs to move beyond historical health care information to include new data sources, including genomics and social media, to aid in research and innovation, says Anna Theriault, director, Business Line Management, Data Solutions, Elekta.
“Oncology EMRs need to move from transaction to workflow-driven systems with integrated decision support,” says Theriault. “They will need to incorporate genetic data with diagnostic information, as an example, to support personalized care.”
Health care interoperability and big data have the potential to improve treatment and, ultimately, patient outcomes, she adds. “To do this, oncology EMRs must be able to integrate with other health care information technology to ensure all of the information is captured, aggregated, and stored in a meaningful way. However, the vast amount of data generated by patients that needs to be incorporated to aid in care delivery and also research and development of new treatment protocols is complex and sometimes incomplete. Current information is captured in disparate systems, which may not have standard communication protocols.”
Compared to traditional EMRs that capture inpatient or outpatient visits, an oncology EMR must also connect multiple points of care across care providers, clinics and departments—laboratory, radiology, genomics, oncologists, therapists, dosimetrists, social workers, etc.
“Oncology EMRs need to be integrated with other systems that have diagnostic, treatment, and follow-up data across the care continuum to ensure the patient treatment is optimized,” Theriault says.
Singh adds, “We need to create a single source of truth about the patient. It’s really about creating a system where everyone has access to the same information from different data sources, with the idea of making data and workflow accessible and collaborative across the team,” he adds. “The term, Internet of Things, is particularly relevant to oncology—how do we bring it all together for a complete picture that connects multiple points of care.”
To achieve this type of integration, standards and open access should apply to data sharing, Singh adds. Similar to the financial industry whereby funds are transferred worldwide across different systems safely and securely, interoperability across oncology systems needs to be a fundamental component of IT and EMRs.
To achieve greater interoperability, Varian is moving beyond the traditional interface engine to web-based application programming interface (API) interoperability with bidirectional and secure exchange of data. The company is also focusing on ways to shorten the benchside-to-bedside cycle. “A big motivator is to continually raise the bar to find new standards of care—we call it a rapid learning cycle,” Singh says.
Varian’s RapidPlan is a knowledge-based planning solution shown to reduce treatment planning time. One study presented at ASTRO 2015 found that IMRT treatment planning time for cervical cancer using a Rapid Plan model based on 86 previously treated cases took an average of 6.85 minutes compared to manual planning that would typically require 2-6 hours of optimization. Singh adds that this study is a key example of combining prior digital knowledge with machine learning to improve outcomes. 1
Elekta is also keenly focused on integration. Theriault explains that MOSAIQ is a comprehensive oncology EMR that incorporates medical and radiation oncology allowing for improved provider collaboration and seamless workflow across the cancer care continuum. MOSAIQ Oncology Analytics integrated with the EMR provides a comprehensive quality outcomes and operational performance management analytics solution.
Key Considerations
While integration and data analytics are key considerations when looking at oncology EMRs, other important considerations require looking inward.
“We are at the mercy of our IT departments,” Dr. Posner says, “so part of that consideration is the IT infrastructure: It’s necessary, and without it you may go nowhere.” This includes an evaluation of existing and planned future systems, networks, and staff. Regarding solutions already in place, there is a difference between compatible and optimized, he adds.
“Both Varian and Elekta have very good quality systems and machines,” he says. For his practice, the big question was the historical data and keeping it on one system vs. going through the often timely and costly endeavor of data migration.
Singh advises that facilities take the time to fully understand their workflows and how it all connects together. “How does data flow from one system to another? Know what you have today and how it will change with a new solution,” he urges.
Don’t underestimate the impact or volume of change management efforts, he adds. “There is a tendency to replicate paper-based workflows in an electronic workflow,” Singh says. “Look at the enterprise to realize the full potential of the technology. That overnight switch of the technology goes well beyond training.”
Theriault also encourages providers and facilities to evaluate how the system can help minimize waste and improve patient-provider collaboration for optimal care.
As Singh reminds, “It takes a village to treat a cancer patient.”
Reference
- Li N, Carmona L, Sirak I, et al. Validation of a knowledge-based automated planning system in cervical cancer as a clinical trial quality system [abstract]. Presented at: American Society for Radiation Oncology (ASTRO) 57th Annual Meeting: October 18-21, 2015; San Antonio, Texas.
Citation
MB M. Oncology EMRs: More than a patient record. Appl Radiat Oncol. 2016;(3):38-40.
September 12, 2016