Radiation Added to Systemic Therapy Extends Survival in Advanced Liver Tumor Patients
 A randomized phase III clinical trial presented at the American Society for Radiation Oncology (ASTRO) 2022 Annual Meeting reported that adding radiation therapy to systemic therapy for patients with advanced liver cancer can extend overall survival and delay tumor progression without compromising patients’ quality of life. Findings from NRG Oncology/RTOG 1112 trial (NCT01730937) indicate that radiation therapy should be a standard treatment option for patients with liver cancer who are ineligible for resection and other standard local-regional therapies.
A randomized phase III clinical trial presented at the American Society for Radiation Oncology (ASTRO) 2022 Annual Meeting reported that adding radiation therapy to systemic therapy for patients with advanced liver cancer can extend overall survival and delay tumor progression without compromising patients’ quality of life. Findings from NRG Oncology/RTOG 1112 trial (NCT01730937) indicate that radiation therapy should be a standard treatment option for patients with liver cancer who are ineligible for resection and other standard local-regional therapies.
“Adding radiation therapy to systemic therapy delayed tumor progression and lengthened survival, without an increase in side effects. In all regards, the combination of radiation therapy and sorafenib appears more effective than the drug on its own,” said Laura A Dawson, MD, FASTRO, lead author of the study, as well as a professor of radiation oncology at the University of Toronto and a practicing radiation oncologist at the Princess Margaret Cancer Centre/University Health Network in Toronto.
Liver cancers are among the most diagnosed cancers and the third leading cause of cancer death worldwide. Incidence rates of hepatocellular carcinoma (HCC), the most common type of liver cancer, in the United States have more than tripled since 1980, and mortality rates have also risen despite the growing availability of screening and improved treatments for the diseases that increase the risk of liver cancer.
Systemic therapy is the standard of care for patients with HCC who are not eligible for surgical resection or other invasive therapies, but a growing number of studies suggest a benefit of radiation therapy for these patients. The trial led by Dr Dawson is the first randomized North American study focused specifically on the role of radiation therapy for these patients.
Participants in the trial included 193 patients (177 eligible for analyses) with new or recurrent advanced HCC who were ineligible for surgical resection or other local or regional standard therapies due to underlying clinical factors or because their cancer had returned after standard therapy. Most patients had invasion of their cancer into the hepatic vasculature (a poor prognostic factor), and a small number had metastases outside of the liver. The median age was 66 years (range 27-84).
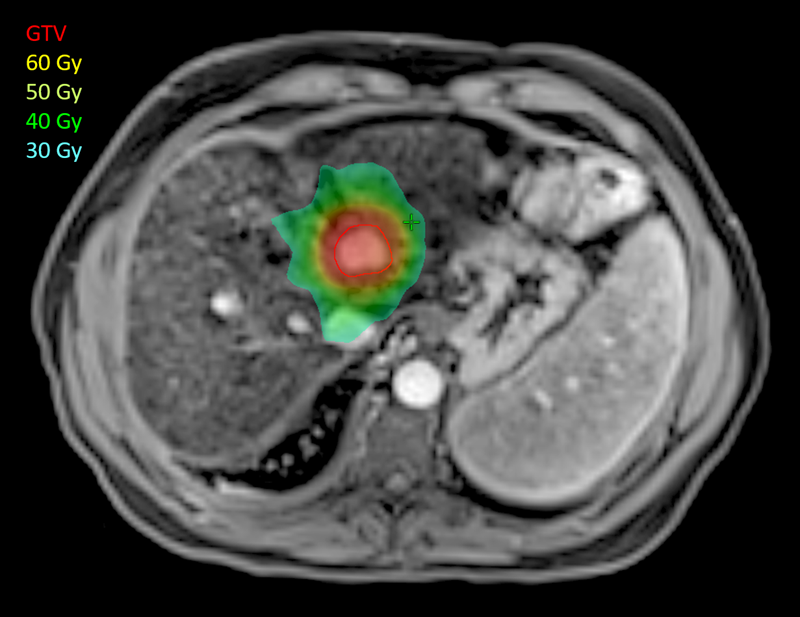
Trial participants were randomized at 23 sites in the US and Canada to receive either sorafenib alone or stereotactic body radiation therapy (SBRT) followed by sorafenib. Sorafenib was the standard systemic therapy when the study began. SBRT was delivered in five fractions over five to ten days, with total doses between 27.5 and 50Gy, individualized to each patient based on clinical factors.
Overall survival was longer for patients who received a combination of SBRT and sorafenib, compared to those on sorafenib alone (15.8 vs. 12.3 months; one-sided p = 0.055). The difference was statistically significant after controlling for clinical prognostic factors such as performance status and the degree of vascular invasion (p=0.042).
“It was a little ambitious to design a study with overall survival as the primary endpoint, but when we designed the trial, there were limited systemic therapies available for these patients, and we had strong signals from earlier research that adding SBRT to sorafenib should improve tumor control and lead to improved survival,” said Dr Dawson. “We can now say without hesitation that radiation therapy is an effective treatment for patients with unresectable liver cancer. Outcomes were better for patients treated with SBRT, despite the planned delay in starting sorafenib.”
Progression-free survival was improved with the addition of SBRT, from 5.5 months with sorafenib alone to 9.2 months with the combination therapy (HR = 0.92, p<0.001). Patients in the combination arm also had longer intervals before their cancers progressed (18.5 vs. 9.5 months; HR = 0.69,
p=0.034).
Treatment-related side effects were not significantly different between the treatment groups. 42% of patients on the sorafenib arm and 47% of patients on the SBRT/sorafenib arm experienced severe (i.e., grade 3 or higher) side effects, and there was one treatment-related death, on the sorafenib-only arm.
While the study was designed to follow patients for five years, Dr Dawson said that she continues to see longer-term benefits in her clinic. “Some patients who had SBRT on the trial are still returning to my clinic more than five years after being treated and doing very well.”
The study was closed to accrual earlier than expected, due primarily to a change in the standard systemic treatment for advanced HCC. Prior to 2016, sorafenib was the only FDA-approved first-line treatment for the disease, but since then, several molecular targeted drugs and more recently, immune checkpoint inhibitors have been adopted into the standard of care.
Dr Dawson said she hopes the findings spark an increased interest in future clinical trials to study the benefit of radiation therapy combined with newer drug therapies. “There is a growing number of preclinical and early clinical studies suggesting that SBRT may be synergistic with immunotherapy, with more than an additive benefit for patients,” she noted.
Other remaining questions include the optimal dosing and sequencing of radiation therapy with different therapies, as well as the potential benefit of radiation alone for patients who are ineligible for standard therapies.