Study Reports Elevated Risk for Ovarian Cancer in Women With Endometriosis
 A landmark study has found that women with severe endometriosis are 10 times more likely to get ovarian cancer, compared to women who do not have the disease. The researchers are from Huntsman Cancer Institute at the University of Utah (the U), the Spencer Fox Eccles School of Medicine at the U, and Boston University Chobanian & Avedisian School of Medicine.
A landmark study has found that women with severe endometriosis are 10 times more likely to get ovarian cancer, compared to women who do not have the disease. The researchers are from Huntsman Cancer Institute at the University of Utah (the U), the Spencer Fox Eccles School of Medicine at the U, and Boston University Chobanian & Avedisian School of Medicine.
Prior studies have shown a causal connection between endometriosis and ovarian cancer. But in using the Utah Population Database—a repository of linked health records housed at Huntsman Cancer Institute—investigators were able to analyze the incidence rates of different types of endometriosis and subtypes of ovarian cancer for the first time.
Their research, which included a cohort of over 78,000 women with endometriosis, has been published in the Journal of the American Medical Association.
“These are really important findings,” says Jennifer Doherty, PhD, MS, investigator and co-leader of the Cancer Control and Population Sciences Program at Huntsman Cancer Institute and professor of the population health sciences department at the U. “This impacts clinical care for individuals with severe endometriosis, since they would benefit from counseling about ovarian cancer risk and prevention. This research will also lead to further studies to understand the mechanisms through which specific types of endometriosis cause different types of ovarian cancer.”
The project began as a collaboration between Doherty, Mollie Barnard, ScD, an assistant professor of medicine at Boston University Chobanian & Avedisian School of Medicine, and Karen Schliep, PhD, MSPH, associate professor of public health at the U. Schliep served as senior and corresponding author of the study.
“Karen [Schliep] was researching endometriosis, and Mollie [Barnard] and I were working on ovarian cancer. We mutually approached each other about putting the data from our two studies together, and that’s how this very powerful combined analysis happened,” says Doherty. “It’s hard to have a large enough study to be able to observe the results we did—all thanks to the Utah Population Database.”
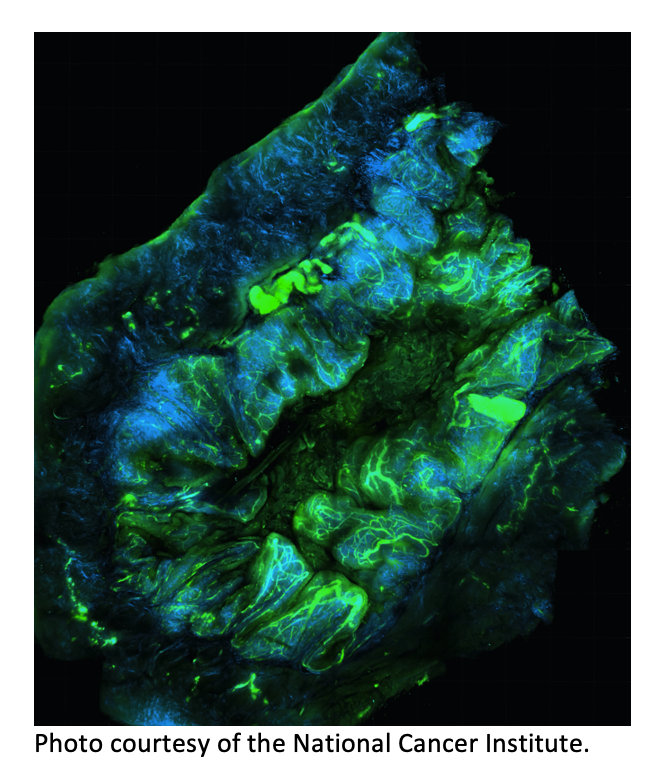
Endometriosis is a disease in which the tissue that lines the uterus grows elsewhere in the pelvic cavity, creating lesions on the ovaries, fallopian tubes, or behind the uterus. An estimated 11% of women in the United States, 6,500,000 in total, have the condition which often leads to chronic pain and infertility.
According to the World Health Organization, the disease presents in three main forms. Superficial endometriosis is mainly seen on the mucous membrane around the pelvic cavity. More severe forms are found as cysts within the ovaries called endometriomas and as deep infiltrating endometriosis, which affects the organs near the uterus, like the ovaries, bladder and bowels.
In the Utah-based cohort, researchers found that women suffering from more severe types of endometriosis are more likely to develop type I ovarian cancer.
“That's where we found a 19-fold increased risk, which compares to the connection between smoking and lung cancer,” says Schliep. “As an epidemiologist, seeing numbers like that is really striking.”
In their calculations, they also found that women with any kind of endometriosis have a 4.2-fold risk of developing ovarian cancer compared to those who do not. They also have over 7 times the risk of developing type I ovarian cancer, which is slow to develop but also does not respond well to chemotherapy.
The National Cancer Institute says that ovarian cancer has a five-year survival rate of 50%.
“The big question for women is ‘what can I do about it?’ This is important data for women to have as they're weighing what kind of treatments they should maybe undergo to avoid any kind of disease down the road,” says Schliep. “I’m very passionate about giving women the right information and then having them be able to make shared decisions with their physician.”
As a preventative measure, women with endometriosis could pursue surgeries including a hysterectomy or removal of the ovaries. But these are invasive procedures, and investigators say more research is needed to know if these are the right measures.
Barnard, a former postdoctoral student at Huntsman Cancer Institute, feels hopeful about the study’s ability to make an impact in women’s lives.
“I chose to become an epidemiologist to make a difference in people's lives, and often we're several steps away from drug development or clinical practice,” says Barnard. “But this feels like it's just a few steps away where it might take just a couple of clinical studies or implementation studies to figure out how this information can best be leveraged by doctors and their patients.”