The Economic Impact of the COVID-19 Pandemic on Radiation Oncology Practice
Images
The coronavirus disease 2019 (COVID-19) has caused economic disruption across the health care system. While much of the literature has focused on the direct costs of preventing and treating COVID-19, the pandemic has also affected the cost of delivering care across the cancer continuum, including in radiation oncology.1 The economics of radiation therapy delivery are impacted by changes in the direct and indirect costs of delivering treatment, reimbursement structures, changes in demand and utilization, and the expected value of treatment. The COVID-19 pandemic has affected these factors on multiple levels: the number of patients seen at cancer centers has been reduced, additional safety procedures have been introduced, the availability and training of personnel has been affected, patient behavior has been influenced, and clinical practice has changed.2-4
The economics of radiation therapy delivery are impacted by changes in the direct and indirect costs of delivering treatment, reimbursement structures, changes in demand and utilization, and the expected value of treatment. The COVID-19 pandemic has affected these factors on multiple levels: the number of patients seen at cancer centers has been reduced, additional safety procedures have been introduced, the availability and training of personnel has been affected, patient behavior has been influenced, and clinical practice has changed.2-4
The economic impact of COVID-19 can be evaluated at different stages of the treatment pathway. The American Association of Physicists in Medicine (AAPM) previously developed a process map that outlines the workflow of each step in radiation oncology practice, which includes the initial patient assessment, treatment planning and delivery, quality assurance, and post-treatment evaluation.5 This process map has been previously applied to characterize the resource requirements and costs of radiation therapy using an activity-based costing approach. The Health Economics in Radiation Oncology program of the European Society of Radiotherapy and Oncology (ESTRO-HERO) adopted this workflow into their time-driven activity-based costing model and organized the activities needed to deliver radiation therapy along 3 activity levels defined as “core” radiation oncology services, “support” services such as departmental management and quality assurance, and activities “beyond” the radiation therapy care pathway such as participation in the multidisciplinary team, long-term follow-up, and survivorship.6
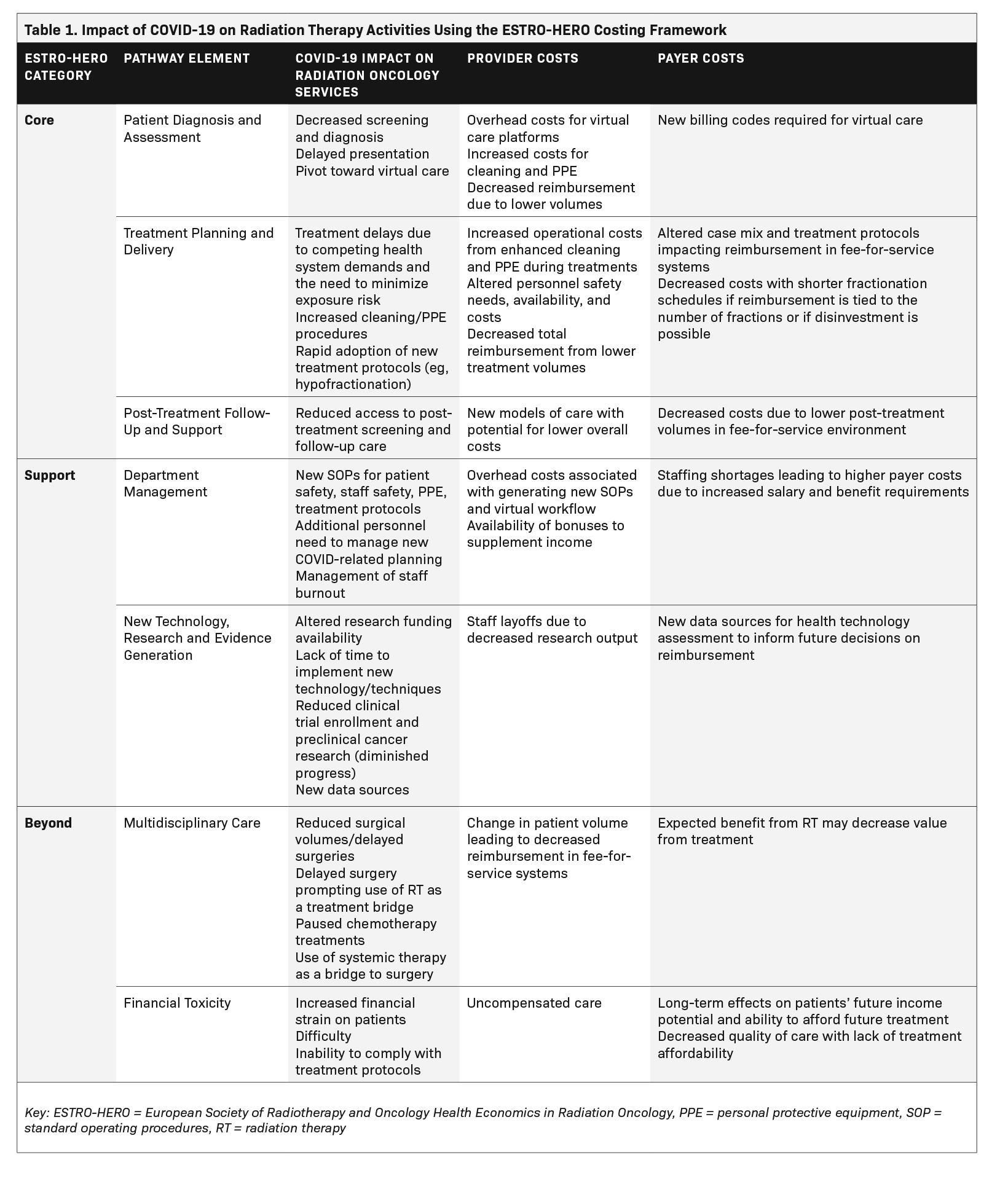
Using the AAPM process map and the ESTRO-HERO costing model as a guide,6 we comprehensively evaluate the economic impact of COVID-19 on radiation oncology from the perspective of the patient, provider, and health care system on core, support, and beyond radiation oncology activities. Although the economic crisis caused by the COVID-19 pandemic was initially thought to be V-shaped with a quick recovery, the pandemic has demonstrated the potential for a W-shape, with relapse due to further lockdowns, or L-shape, with a more permanent loss of output.7 Understanding the economic impact of COVID-19 on the practice of radiation oncology is critical to mitigate ongoing perturbations on patients, providers, and clinical practices due to the current pandemic as well as future health care shocks, to ensure evidence-based resource allocation, and to identify opportunities for innovation to support value-based care.
Economic Impact on Core Radiation Oncology Activities
Core activities in radiation oncology can be grouped into 3 key activity areas along the patient care pathway: 1) patient diagnosis and assessment, 2) treatment planning and delivery, and 3) post-treatment management. These activity areas have been adapted and broadened from the original ESTRO-HERO framework to include activities directly impacting radiation oncologists’ time, costs, and reimbursement. Each of these activity areas is affected by changes in capital and operational costs as well as reimbursement. Capital costs include the upfront investment in equipment, facilities, and training of personnel, whereas operational costs are related to the utilization of equipment (treatment-related costs and quality assurance), staffing (including continuing education of personnel) and maintenance (including building and machinery maintenance and overhead). The impact of COVID-19 on cost and reimbursement at each of these time points is shown in Table 1. Although costs and reimbursement should be linked, costs reflect the quantity and quality of consumed resources, while reimbursement reflects society’s agreement to pay for a health care service and is negotiated between providers and payers.8 The structure and type of reimbursement systems vary between countries, with differences in the components of radiation treatment that are eligible for reimbursement, the fees paid for treatment techniques, fractionation schedules, and indications.9
Patient Diagnosis and Assessment
Screening and diagnostic services for cancer were significantly reduced over the course of the COVID-19 pandemic due to increased demands on the health care system as well as public health messaging to seek care only when urgently required to minimize contact and mitigate risk.10-13 Patient behaviors also changed, with many postponing or forgoing screening or diagnostic investigations due to fear of contracting COVID-19. A cross-sectional study from January 2018 to March 2021 in the US found that the number of weekly new cases of breast, prostate, colorectal, pancreatic, gastric, and esophageal cancer declined by 46.4% overall during the first year of the pandemic, ranging from 24.7% for pancreatic cancer to 51.8% for breast cancer.14 This combination of reduced availability and demand for screening and diagnostic services had a significant downstream impact on demand for radiation therapy, the complexity of treatment, and on provider and facility revenue.
A survey by the American Society for Radiation Oncology (ASTRO) in April 2020 of 222 leaders in academic and community practices in the US on the initial impact of the COVID-19 pandemic found that 81% of practices reported a reduction in referrals and that, on average, practices reported treating 68% of their usual volume (range: 10% to 95%).15 Practices also reported some decrease in monthly revenue, with 71% of practices estimating revenue declines of 20% or more. In specialized centers, reduced patient flow and postponed treatments had a particularly negative impact on the return on investment of recently introduced high-cost interventions such as MR-linac or proton-beam radiation therapy, as their cost could not be buffered by other treatments already established in the department.2,15 Some departments in the US noted a decline in billable activity of up to 35%, driven by a significant decline in the demand for consultation and treatment.16 By the end of 2020, Medicare physician fee schedule services had declined by 8% overall, compared with the same period prior to the pandemic.17
The ASTRO survey was also sent to European department heads in May 2020 and similar findings were observed, with 60% of clinics reporting a decline in patient volume.18 In February 2021, after 1 year of the COVID pandemic, ESTRO repeated the survey and noted an improvement in demand for treatment, but a persistent decrease in 53% of the centers surveyed in patient volume compared with before the pandemic.18 In Latin America, initial consultations were reduced by 28% to 38%, with a corresponding reduction in pathology (6% to 50%), cancer surgery (28% to 70%), and chemotherapy (2% to 54%). Reductions in radiation therapy use were noted in Brazil, Chile and Peru (8% to 31%).19
Staffing shortages during the pandemic compounded the impact of fluctuating patient volumes. A survey of radiation therapy department managers from Canada and Norway found that 25% and 39% of departments, respectively, experienced shortages, which were partially due to staff redeployment.20 In Africa, the highest rates of staff shortages were in low-income countries as compared with middle-income countries, which were driven by fear of contracting the virus and inadequate personal protective equipment (PPE).21 In the US, the Coronavirus Aid, Relief, and Economic Security (CARES) Act that was signed into law in March 2020 was intended to offset the loss of revenue of hospitals and clinics and avoid layoffs.22 However, the extent to which this was successful in mitigating staff turnover has not yet been quantified.
In order to further limit interruptions in the delivery of radiation oncology services while maintaining physical distancing, the use of telehealth rapidly increased during the pandemic.23-25 Many radiation oncology services were not previously reimbursed, or adequately reimbursed, through virtual platforms, and the deregulation of telehealth services and the introduction of new temporary fee codes were used to facilitate virtual care.23,26,27 Although in-person visits increased over time with increasing vaccination rates, the demand for virtual options by both patients and providers has prompted shifts in the regulatory landscape and the more permanent integration of telehealth into routine practice.28 Future work will need to evaluate the appropriateness of virtual care in different clinical scenarios and the relative value of this service.
Treatment Planning and Delivery
During the early phase of the pandemic, recommendations to delay or omit radiation treatment to minimize COVID-19 exposure risk contributed to the reduction in revenue for clinical departments.29,30 For example, omission of radiation therapy with active surveillance was considered a reasonable option for low- and favorable intermediate-risk prostate cancer, whereas delaying radiation through the use of prolonged androgen deprivation therapy of up to 6 to 7 months was acceptable for higher-risk disease.30,31 For other types of cancer, however, radiation therapy was used as a bridging measure to delay procedures that might be associated with a higher COVID-19 risk or as an alternative treatment option. For example, international experts recommended that short courses of radiation therapy could be used to delay surgery in patients with rectal cancer.32 In lung cancer, an ESTRO-ASTRO consensus statement recommended the use of stereotactic radiation for patients with operable early stage non-small cell lung cancers in cases where timely access to surgery was unavailable due to surgical capacity issues.33 This shift in practice is supported by data from the UK that found an increase in the number of radiation therapy courses during the initial months of the pandemic for esophageal, bladder, and rectal cancer, which may reflect the greater use of radiation therapy as an alternative to surgery.34 These changes to case mix and treatment protocols led to unexpected shifts in department resource allocation, altering departmental costs, reimbursements and human resource needs.34
The COVID-19 pandemic also led to the rapid adoption of hypofractionated or accelerated treatment schedules,3,35 where radiation is delivered at a higher dose over fewer treatments, to minimize patient exposure and maximize treatment unit efficiency.30 There has been growing interest in using hypofractionation over the last several years to increase machine availability, reduce resource consumption, and improve patient convenience. In the fee-for-service setting, however, where remuneration has been tied to the number of fractions delivered, uptake on hypofractionation had been slow, despite the strong evidence base in several indications.9,36 In contrast to historical hypofractionation utilization rates, COVID-19 prompted the rapid adoption of hypofractionated schedules, which were endorsed by multiple professional societies. For example, the FAST-Forward trial published in April 2020 found that a 1-week course of adjuvant radiation therapy for early stage breast cancer at a dose of 26 Gy in 5 fractions was noninferior to moderate hypofractionation delivered over 3 weeks in terms of ipsilateral breast tumor relapse and normal tissue effects.37 This fractionation scheme was widely adopted in international centers following its publication38 and was established as a standard of care at a U.K. consensus meeting in October 2020.39 A cost-minimization analysis in the Canadian context found that implementation of FAST-Forward results in a 36% reduction in infrastructure and human resource costs compared with standard fractionation, which translated to an annual savings of over $2 million Canadian dollars (CAD) per year at the provincial level and $174,700 per year at the institutional level.40 However, these savings require flexibility in equipment and personnel costs, which are sometimes fixed at the departmental level. A transition to hypofractionated schedules was suggested as a safe strategy for several other curative and palliative radiation therapy indications.30,41
Post-treatment
Once treatment has been completed, patients require ongoing surveillance for recurrence, and monitoring for radiation-related toxicities. COVID-19 made surveillance for disease recurrence more challenging to access, particularly as health resources were diverted towards management of the pandemic, and follow-up assessments to evaluate for disease recurrence or residual toxicities were increasingly done virtually.42 The Multinational Association of Supportive Care in Cancer Survivorship Group conducted a qualitative survey of their membership to evaluate how members and their respective institutions have modified cancer survivorship practices and services during COVID-19.43 One of the priority areas to emerge from this survey was the opportunity for cancer care practitioners to decentralize or delegate care from the specialist setting. These may include alternative models of care such as shared care or nurse or primary care provider-led models, which would allow oncologists to provide a greater focus on acute patients requiring urgent care.43 The opportunity to implement these new models of care has refocused attention on opportunities for improving value-based care delivery in which high-quality care can be delivered in lower-cost settings.44
Economic Impact on Radiation Oncology Support Activities
Numerous supportive activities are essential for any functioning radiation oncology service, including departmental management, implementation of new technology, research, and evidence generation. COVID-19 impacted each of these areas through reduced staffing availability, funding challenges, and new operating procedures, but also led to a renewed commitment to invest in high-quality real-world data systems and randomized controlled trials to guide practice.
Departmental Management
Radiation oncology departments were required to rapidly adapt their standard operating procedures (SOP) and workflows to ensure the safe provision of treatment during the pandemic. One survey of 68 radiation oncologists across 13 countries found that modifications were made to treatment protocols in 85% of cases.45 This resulted in unexpected overhead costs related to the development of new SOP documents for
style="padding-left: 5pt;text-indent: 0pt;text-align: left;">patient management, screening and cleaning procedures, treatment procedures, safe work practices, PPE guidelines, rules for staff quarantine and isolation and work-from-home guidelines.46 The use of telemedicine also impacted the cost of care delivery due to the need for new information systems and online workflows to support virtual encounters,47 although it led to significant indirect cost savings through reduced travel costs and patient time away from work.23,48
Operational costs also increased due to greater personnel needs and training, consumables such as masks and PPE, increased treatment times due to cleaning procedures and potentially slower patient setup while wearing PPE.2 There were also additional overhead costs for plexiglass and other physical barriers at screening and registration desks.49 Further, burnout from the COVID pandemic has also been well- documented to affect productivity and the challenges with family support and childcare (eg, high-risk elderly parents, closed schools), and employee sick leave due to COVID-19-related illness or quarantine requirements have all affected departmental staffing and efficiency. In some US jurisdictions, the staffing challenges have led to higher costs related to hazard pay, salary increases, signing bonuses and improved benefits packages.50
Implementation of New Technology, Research and Evidence Generation
Evidence generation is essential for making better choices about health care and health care funding. The impact of the pandemic on the field of evidence generation has been mixed. Prior to the pandemic, the lack of real-time and real-world evidence slowed the uptake of new and beneficial advances and has often resulted in ineffective, costly, or even harmful interventions remaining in clinical use.51 However, COVID-19 has highlighted the importance and need for population databases, resulting in increased investment in this important research area. New consortia to rapidly address cancer-specific research questions were developed, such as the COVID-19 and Cancer Consortium (CCC19), which aims to bridge the knowledge gap in cancer care caused by the COVID-19 pandemic.52 Several other registries and consortia to support real-world data collection on cancer and COVID have emerged internationally, many of which are spearheaded by professional societies such as the American Society of Clinical Oncology (ASCO), European Society for Medical Oncology COVID-19 Care (ESMOCoCare), and the European Organization for Research and Treatment of Cancer (EORTC) E2 -RADIatE.53 Such data can contribute to more robust health technology assessment in cancer and improved evaluation of the magnitude of benefit and cost-effectiveness of radiation therapy interventions.
A major challenge in evidence generation during the first year of the pandemic, however, was the dramatic reduction in enrollment in clinical trials in oncology, collection of patient samples for cancer research, and preclinical bench work.46 The scale-up of clinical trial activity following the initial shutdown, however, provided an opportunity to evaluate which components of clinical trials were necessary to reach the goal of testing the effectiveness of cancer therapy. Such changes have the potential to improve the benefit that patients are receiving from participation and reduce unnecessary visits.55 Funding opportunities also changed, with a reduction in opportunities for non-COVID research, as research budgets for cancer were reduced to shift funds toward COVID-related research activities. The Association of Medical Research Charities estimated a £252 to 368 million shortfall in research investment in 2020-202156 and similar declines in funding availability have been seen globally.57
Economic Impact on Activities Beyond Radiation Oncology
Beyond the treatment of the disease itself, many other aspects of care delivery, including surgery, systemic treatment, supportive care, and rehabilitation have all been affected by the pandemic. In England, premature cancer deaths resulting from diagnostic delays from breast, colorectal, esophageal, and lung cancer during the first wave of the pandemic are estimated to amount to a loss of 32,700 quality-adjusted life years and productivity losses of £103.8 million GBP.58 Further, the economic strain experienced by patients in other aspects of their personal lives during the pandemic has implications for outcomes and compliance with treatment. There is growing literature on the burden of financial toxicity that patients experience, which includes the objective financial burden of cancer treatment as well as subjective financial distress. Loss of income and prolonged unemployment from the pandemic created a double financial burden for many patients.59
Conclusion
The COVID-19 pandemic has led to many changes in radiation therapy delivery, which have impacted the economics of radiation oncology care. While some of these changes, such as the reduction in clinical volume and increased need for PPE, may be temporary during periods of increased COVID-19 infection, others such as the use of virtual care and hypofractionation may lead to more permanent changes.
These changes require ongoing evaluation and monitoring and may prompt payers and health systems to consider new and more flexible reimbursement models. A renewed emphasis on evidence generation, which was motivated by the pandemic, may facilitate more robust and timely health technology evaluation of new models of care and new innovation in treatment.
References
- Shubber N, Sheppard J, Alradhawi M, Ali Y. The impacts of the novel SARS-CoV-2 outbreak on surgical oncology - a letter to the editor on “The socio-economic implications of the coronavirus and COVID-19 pandemic: a review.” Int J Surg. 2020;79:109-110.
- Appel S, Kaidar-Person O, Lawrence YR, et al. The Coronavirus pandemic in Israel: implications for radiation oncology departments. Isr Med Assoc J. 2020;22(4):211-213.
- Weisel KC, Morgner-Miehlke A, Petersen C, et al. Implications of SARS-CoV-2 infection and COVID-19 crisis on clinical cancer care: report of the University Cancer Center Hamburg. Oncol Res Treat. 2020;43(6):307-313.
- Broom A, Kenny K, Page A, et al. The paradoxical effects of COVID-19 on cancer care: current context and potential lasting impacts. Clin Cancer Res. 2020;26(22):5809-5813.
- Ford EC, Fong de Los Santos L, Pawlicki T, Sutlief S, Dunscombe P. Consensus recommendations for incident learning database structures in radiation oncology. Med Phys.2012;39(12):7272-7290.
- Defourny N, Perrier L, Borras JM, et al. National costs and resource requirements of external beam radiotherapy: a time-driven activity-based costing model from the ESTRO-HERO project. Radiother Oncol. 2019;138:187-194.
- Sharma D, Bouchaud JP, Gualdi S, Tarzia M, Zamponi F. V-, U-, L- or W-shaped economic recovery after Covid-19: insights from an agent based model. PLoS One. 2021;16(3):e0247823.
- Defourny N, Dunscombe P, Perrier L, Grau C, Lievens Y. Cost evaluations of radiotherapy: What do we know? An ESTRO-HERO analysis. Radiother Oncol. 2016;121(3):468-474.
- Lievens Y, Defourny N, Corral J, et al. How public health services pay for radiotherapy in Europe: an ESTRO-HERO analysis of reimbursement. Lancet Oncol. 2020;21(1):e42-e54.
- Skovlund CW, Friis S, Dehlendorff C, Nilbert MC, Morch LS. Hidden morbidities: drop in cancer diagnoses during the COVID-19 pandemic in Denmark. Acta Oncol.2021;60(1):20-23.
- Jacob L, Loosen SH, Kalder M, Luedde T, Roderburg C, Kostev K. Impact of the COVID-19 pandemic on cancer diagnoses in general and specialized practices in Germany. Cancers (Basel). 2021;13(3).
- Morris EJA, Goldacre R, Spata E, et al. Impact of the COVID-19 pandemic on the detection and management of colorectal cancer in England: a population-based study. Lancet Gastroenterol Hepatol. 2021;6(3):199-208.
- Fedewa SA, Cotter MM, Wehling KA, Wysocki K, Killewald R, Makaroff L. Changes in breast cancer screening rates among 32 community health centers during the COVID-19 pandemic. Cancer. 2021.
- Kaufman HW, Chen Z, Niles J, Fesko Y. Changes in the number of us patients with newly identified cancer before and during the coronavirus disease 2019 (COVID-19) pandemic. JAMA Netw Open. 2020;3(8):e2017267.
- Wakefield DV, Sanders T, Wilson E, et al. Initial impact and operational responses to the COVID-19 pandemic by American radiation oncology practices. Int J Radiat Oncol Biol Phys. 2020;108(2):356-361.
- Goenka A, Ma D, Teckie S, et al. Implementation of telehealth in radiation oncology: rapid integration during Covid-19 and its future role in our practice. Adv Radiat Oncol. 2021;6(1):100575.
- Gillis K. Impacts of the COVID-19 Pandemic on 2020 Medicare Physician Spending. American Medical Association. Policy Research Perspectives Web site. https://www. ama-assn.org/system/files/2020-prp-covid-impact-medicare-physician-spending.pdf. Published 2021. Accessed December 10, 2021.
- Slotman BJ, Lievens Y, Poortmans P, et al. Effect of COVID-19 pandemic on practice in European radiation oncology centers. Radiother Oncol. 2020;150:40-42.
- Vázquez Rosas T, Cazap E, Delgado L, et al. Social distancing and economic crisis during Covid-19 pandemic reduced cancer control in latin america and will result in increased late-stage diagnoses and expense. JCO Glob Oncol. 2021;7:694-703.
- Morassaei S, Di Prospero L, Ringdalen E, et al. A survey to explore the psychological impact of the COVID-19 pandemic on radiation therapists in Norway and Canada: a tale of two countries. J Med Radiat Sci. 2021;68(4):407-417.
- Martei YM, Rick TJ, Fadelu T, et al. Impact of COVID-19 on cancer care delivery in Africa: a cross-sectional survey of oncology providers in Africa. JCO Glob Oncol. 2021;7:368-377.
- CARES Act Provider Relief Fund. US Department of Health and Human Services. https://www.hrsa.gov/provider-relief/. Updated April 10, 2020. Accessed December 10, 2021.
- Berlin A, Lovas M, Truong T, et al. Implementation and outcomes of virtual care across a tertiary cancer center during COVID-19. JAMA Oncol. 2021;7(4):597-602.
- Weiner JP, Bandeian S, Hatef E, Lans D, Liu A, Lemke KW. In-person and telehealth ambulatory contacts and costs in a large US insured cohort before and during the Covid-19 pandemic. JAMA Netw Open. 2021;4(3):e212618.
- Lieneck C, Garvey J, Collins C, Graham D, Loving C, Pearson R. Rapid telehealth implementation during the Covid-19 global pandemic: a rapid review. Healthcare (Basel). 2020;8(4).
- (ASPA) ASfPA. Telehealth: delivering care safely during COVID-19. U.S. Department of Health & Human Services. https://www.hhs.gov/coronavirus/telehealth/index.html. Published 2021. Updated July 15, 2020. Accessed October 3, 2021, 2021.
- Physician billing codes in response to COVID-19. Canadian Institute for Health Information. https://www.cihi.ca/en/physician-billing-codes-in-response-to-covid-19. Published 2021. Updated August 19, 2021. Accessed October 3, 2021, 2021.
- Royce TJ, Sanoff HK, Rewari A. Telemedicine for cancer care in the time of COVID-19. JAMA Oncol. 2020;6(11):1698-1699.
- Zaniboni A, Ghidini M, Grossi F, et al. A review of clinical practice guidelines and treatment recommendations for cancer care in the COVID-19 pandemic. Cancers (Basel). 2020;12(9).
- Simcock R, Thomas TV, Estes C, et al. COVID-19: Global radiation oncology’s targeted response for pandemic preparedness. Clin Transl Radiat Oncol. 2020;22:55-68.
- Zaorsky NG, Yu JB, McBride SM, et al. Prostate cancer radiation therapy recommendations in response to COVID-19. Adv Radiat Oncol. 2020;5(4):659-665.
- Marijnen CAM, Peters FP, Rödel C, et al. International expert consensus statement regarding radiotherapy treatment options for rectal cancer during the COVID 19 pandemic. Radiother Oncol. 2020;148:213-215.
- Guckenberger M, Belka C, Bezjak A, et al. Practice recommendations for lung cancer radiotherapy during the COVID-19 pandemic: an ESTRO-ASTRO Consensus Statement. Int J Radiat Oncol Biol Phys. 2020;107(4):631-640.
- Spencer K, Jones CM, Girdler R, et al. The impact of the COVID-19 pandemic on radiotherapy services in England, UK: a population-based study. Lancet Oncol. 2021;22(3):309-320.
- Akuamoa-Boateng D, Wegen S, Ferdinandus J, Marksteder R, Baues C, Marnitz S. Managing patient flows in radiation oncology during the COVID-19 pandemic: Reworking existing treatment designs to prevent infections at a German hot spot area University Hospital. Strahlenther Onkol. 2020;196(12):1080-1085.
- Rodin D, Tawk B, Mohamad O, et al. Hypofractionated radiotherapy in the real-world setting: an international ESTRO-GIRO survey. Radiother Oncol. 2021;157:32-39.
- Murray Brunt A, Haviland JS, Wheatley DA, et al. Hypofractionated breast radiotherapy for 1 week versus 3 weeks (FAST-Forward): 5-year efficacy and late normal tissue effects results from a multicentre, non-inferiority, randomised, phase 3 trial. Lancet. 2020;395(10237):1613-1626.
- Koch CA, Lee G, Liu ZA, et al. Rapid adaptation of breast radiation therapy use during the coronavirus disease 2019 pandemic at a large academic cancer center in Canada. Adv Radiat Oncol. 2020;5(4):749-756.
- Obeng-Gyasi S, Coles CE, Jones J, et al. When the world throws you a curve ball: lessons learned in breast cancer management. Am Soc Clin Oncol Educ Book. 2021;41:1-11.
- Yaremko HL, Locke GE, Chow R, Lock M, Dinniwell R, Yaremko BP. Cost minimization analysis of hypofractionated radiotherapy. Curr Oncol. 2021;28(1):716-725.
- Widmark A, Gunnlaugsson A, Beckman L, et al. Ultra-hypofractionated versus conventionally fractionated radiotherapy for prostate cancer: 5-year outcomes of the HYPO-RT-PC randomised, non-inferiority, phase 3 trial. Lancet. 2019;394(10196):385-395.
- Archer S, Holch P, Armes J, et al. “No turning back” psycho-oncology in the time of COVID-19: insights from a survey of UK professionals. Psychooncology. 2020;29(9):1430-1435.
- Nekhlyudov L, Duijts S, Hudson SV, et al. Addressing the needs of cancer survivors during the COVID-19 pandemic. J Cancer Surviv. 2020;14(5):601-606.
- Blumenthal D, Fowler EJ, Abrams M, Collins SR. Covid-19 - Implications for the health care system. N Engl J Med. 2020;383(15):1483-1488.
- Appel S, Lawrence YR, Symon Z, Kaidar-Person O. COVID-RO study: the radiation oncology practice at times of COVID-19 outbreak - international survey. Rep Pract Oncol Radiother. 2021;26(1):20-28.
- Chaudhari S, Sharma SD, Shrivastava SK. Revision in standard operating procedures of radiation oncology department and quality assurance schedule under COVID-19 pandemic. J Med Phys. 2020;45(2):130-133.
- Rodin D, Lovas M, Berlin A. The reality of virtual care: implications for cancer care beyond the pandemic. Healthc (Amst). 2020;8(4):100480.
- Abimbola S, Keelan S, Everett M, et al. The medium, the message and the measure: a theory-driven review on the value of telehealth as a patient-facing digital health innovation. Health Econ Rev. 2019;9(1):21.
- Cinar P, Bold R, Bosslet BA, et al. Planning for post-pandemic cancer care delivery: recovery or opportunity for redesign? CA Cancer J Clin. 2021;71(1):34-46.
- Ruhnke GW. Physician supply during the coronavirus disease 2019 (COVID-19) crisis: the role of hazard pay. J Gen Intern Med. 2020;35(8):2433-2434.
- Califf RM, Robb MA, Bindman AB, et al. Transforming evidence generation to support health and health care decisions. N Engl J Med. 2016;375(24):2395-2400.
- Rubinstein SM, Steinharter JA, Warner J, Rini BI, Peters S, Choueiri TK. The COVID-19 and Cancer Consortium: a collaborative effort to understand the effects of Covid-19 on patients with cancer. Cancer Cell. 2020;37(6):738-741.
- Desai A, Mohammed TJ, Duma N, et al. COVID-19 and cancer: a review of the registry-based pandemic response. JAMA Oncol. 2021.
- Mulholland EJ. Impact of COVID-19 on in vivo work and patient sample availability for cancer research. Nat Rev Cancer. 2021;21(3):139-140.
- Flaherty KT, Doroshow JH, Galbraith S, et al. Rethinking cancer clinical trial conduct induced by COVID-19: an academic center, industry, government, and regulatory agency perspective. Cancer Discov. 2021;11(8):1881-1885.
- COVID-19: The risk to AMRC charities. https://www.amrc.org.uk/covid-19-the-risk-to-amrc-charities. Updated 11 June 2020. Accessed September 1, 2021.
- Tsagakis I, Papatriantafyllou M. Safeguarding cancer research funding by European charities amidst the COVID-19 pandemic. Mol Oncol. 2020;14(12):2987-2993.
- Gheorghe A, Maringe C, Spice J, et al. Economic impact of avoidable cancer deaths caused by diagnostic delay during the COVID-19 pandemic: a national population- based modelling study in England, UK. Eur J Cancer. 2021;152:233-242.
- Kong YC, Sakti VV, Sullivan R, Bhoo-Pathy N. Cancer and COVID-19: economic impact on households in Southeast Asia. Ecancermedicalscience. 2020;14:1134.
Citation
. The Economic Impact of the COVID-19 Pandemic on Radiation Oncology Practice. Appl Rad Oncol. 2021;(4):11-17.
December 28, 2021
