Travel-Related Environmental Impact of Telemedicine in a Radiation Oncology Clinic
Affiliations
- Penn Medicine Lancaster General Health, Lancaster, PA
- Ann B. Barshinger Cancer Institute, Lancaster, PA
- Department of Radiation Oncology, Stanford University, Palo Alto, CA
- Department of Radiation Oncology, University of California-San Francisco, San Francisco, CA
Abstract
Objective:
The environmental impact of telemedicine within radiation oncology has not yet been established. This is particularly relevant as climate change is recognized as one of the largest threats to human health, including oncological outcomes. The health care sector significantly contributes to global carbon emissions, in part due to patient travel. We assessed the impact of telemedicine utilization on patient travel-related greenhouse gas (GHG) emissions for a large radiation oncology clinic located in a densely populated suburban setting.
Materials and Methods:
All in-person and telemedicine visits scheduled in a radiation oncology clinic over 7 consecutive days in June 2021 were retrospectively reviewed. Care visits with out-of-state patients were excluded. Travel distance between patients’ reported home address and the clinic address was estimated using Google Maps. Associated GHG emissions were calculated using a well-to-wheel model. Gas, hybrid, plug-in hybrid, and electric vehicle utilization were accounted for per statewide vehicle registration statistics. GHG emissions were converted into carbon dioxide equivalents (CO2e) using 100-year global warming potentials.
Results:
A total of 156 clinic visits were conducted over the time period; 115 via telemedicine (74%) and 41 in-person (26%). Patients traveling for in-person visits had a median round trip of 44 miles; of those seen via telemedicine, a median of 60 travel miles were saved. Use of telemedicine “saved” an estimated 13,828 travel miles in 1 week, translating into 719,056 miles saved annually. The forecasted annual savings of CO2e attributed to telemedicine visits is 339.8 metric tons, the equivalent emissions of 65.7 homes’ electricity use for 1 year.
Conclusion:
Integration of telemedicine within a radiation oncology clinic reduces the environmental impact of patient care. Advocacy efforts should support telemedicine where feasible and clinically appropriate to decrease carbon emissions associated with the practice of radiation oncology, as well as to establish and promote environmentally sustainable behaviors within the field.
Introduction
Climate change is recognized as one of the largest threats to human health, including oncological outcomes.1 However, the health care sector significantly contributes to global carbon emissions. In fact, if the global health care sector were a country, it would be the fifth largest emitter of greenhouse gas (GHG) emissions worldwide.2 Across the health care system, patient and provider transportation-associated GHG emissions account for a significant portion of total emissions. At our institution alone, patient transportation-associated GHG emissions accounted for the largest proportion (75%) of nonsupply chain scope 3 GHG emissions in 2021.3
Patients with cancer undergo many appointments across the cancer control continuum, including cancer prevention, screening, diagnosis, treatment, and follow-up care.4 Radiation oncology in particular requires many in-person visits to coordinate initial evaluation, work-up, treatment, planning, and delivery. The impact of climate change on oncology is just beginning to be understood and often stems from the disruption of the complex health care systems required for multiple aforementioned stages of cancer care. We postulate that altering the transportation behavior of the cancer patient population where possible would have a measurable impact on reducing health care-associated GHG emissions both due to the frequent visits required for optimal treatment and prevalence of cancer in the United States.
Like many others, our radiation oncology department was forced to rapidly integrate telemedicine into practice in response to the COVID-19 pandemic such that patients could communicate with their health care provider remotely. While there has been an investigation into the implementation, effectiveness, cost, and perceptions of telemedicine, the environmental impact of telemedicine within radiation oncology has not yet been established.5 - 7 In light of recent national regulations pertaining to the use of telemedicine, it is imperative to fully understand the potential benefits and limitations of its use. The aim of this study was to assess the impact of telemedicine on transportation-related GHG emissions for a large, academic radiation oncology outpatient clinic located in a densely populated suburban setting.
Materials and Methods
In-person and telemedicine visits scheduled in our clinic over a consecutive 7-day period in June 2021 were retrospectively reviewed. This time period was selected as COVID cases were at a lull and institutional isolation protocols did not restrict access to in-person visits for those without signs or symptoms of COVID. We define telemedicine as the provision of remote clinical services via real-time two-way communication between patient and health care provider with use of an interactive audiovisual platform. Our institution utilized the VidyoHealth integration with the Epic electronic medical record for telemedicine visits. Visits audited included both new patient consultations and return patient follow-up visits; care visits with patients who resided outside of the state were excluded as well as radiation therapy treatment appointments, as in-person attendance is requisite for treatment. The shortest possible travel distance between patients’ reported home address in the electronic medical record and our clinic address was estimated using Google Maps.8 As our institution is in a densely populated suburb with limited public transportation accessibility, the analysis was based on patient travel assuming a commute by single-occupancy motor vehicle. Vehicle-related GHG emissions were calculated with the publicly available Greenhouse Gases, Regulated Emissions, and Energy Use in Transportation tool using a well-to-wheel model, which accounts for all emissions related to fuel (ie, gas, electricity) production and use.9 Gas, hybrid, plug-in hybrid, and electric vehicle utilization were accounted for per published statewide vehicle registration statistics.10 GHG emissions were converted into carbon dioxide equivalents (CO2e) using 100-year global warming potentials (GWPs).11 GWPs describe the relative potency of a GHG taking account of how long it remains active in the atmosphere and allows comparison of the global warming impact of different GHGs. Annual projections were calculated by multiplying weekly travel distance by 52 weeks. Area Deprivation Index (ADI, a composite measure of socioeconomic disadvantage) scores were obtained for each patient and analyzed per quartile; a higher quartile rank represents a greater disadvantaged block group.12 Chi-square and simple t -test analyses were performed for proportional and continuous variable comparisons, respectively.
Results
A total of 156 clinic visits were conducted over a 7 days. Telemedicine was utilized similarly across gender, race, ethnicity, and insurance status ( Table 1 ). Patients who utilized telemedicine were younger than those who attended in-person visits (mean, 61 years vs 68 years, respectively, P = .03) ( Table 1 ).
Patient Demographics by Visit Encounter Type
| TELEMEDICINE (n = 115) | IN-PERSON (n = 41) | TOTAL | P VALUE | |
|---|---|---|---|---|
| Age, mean | 61 y | 68 y | 63 y | .03 |
| Gender, n (%) | .56 | |||
| Male | 51 (49%) | 21 (44%) | 72 (47%) | |
| Female | 66 (51%) | 22 (56%) | 88 (53%) | |
| Race, n (%) | .67 | |||
| Caucasian | 65 (57%) | 27 (66%) | 92 (59%) | |
| Asian | 23 (20%) | 8 (20%) | 31 (20%) | |
| Black or African American | 3 (3%) | 0 (0%) | 3 (2%) | |
| Other | 24 (21%) | 6 (15%) | 30 (19%) | |
| Ethnicity, n (%) | .63 | |||
| Non-Hispanic/non-Latino | 97 (84%) | 34 (83%) | ||
| Hispanic/Latino | 16 (14%) | 7 (17%) | ||
| Insurance status, n (%) | .86 | |||
| Private | 40 (35%) | 13 (32%) | 53 (34%) | |
| Medicare | 66 (57%) | 23 (56%) | 89 (57%) | |
| Medical | 5 (4%) | 3 (7%) | 8 (5.1%) | |
| Other | 4 (3.5%) | 2 (4.9%) | 6 (3.9%) |
Out of the total 156 clinic visits that occurred over this 1-week span, 115 (74%) were via telemedicine and 41 (26%) were in-person. For new patient visits (n = 55), 8 (15%) were in-person and 47 (85%) were via telehealth. For follow-up visits (n = 101), 33 (33%) were in-person and 68 (67%) were via telehealth.
The use of telemedicine varied by disease site and visit type, as demonstrated in Table 2 . The majority of disease sites utilized telemedicine for new patient visits, with the exception of head and neck new patient consultations, who were exclusively seen in-person. In follow-up, the proportion of in-person visits increased compared with new patient visits, with nearly half of all breast, thoracic, gynecological, and head and neck visits conducted in-person. There was a trend for genitourinary, gastrointestinal, benign, and other sites (sarcoma, cutaneous, pediatric, and lymphoma) to be seen in follow-up via telemedicine ( P = .09).
Visit Type Stratified by Telemedicine Status and Primary Cancer Site
| NEW PATIENT VISITS (n = 55) | FOLLOW-UP VISITS (n = 101) | |||
|---|---|---|---|---|
| IN-PERSONn (%) | TELEMEDICINEn (%) | IN-PERSONn (%) | TELEMEDICINEn (%) | |
| Breast | 0 (0%) | 8 (100%) | 8 (44%) | 10 (56%) |
| Genitourinary | 1 (25%) | 3 (75%) | 3 (20%) | 12 (80%) |
| Thoracic | 1 (11%) | 8 (89%) | 7 (47%) | 8 (53%) |
| Gastrointestinal | 2 (25%) | 6 (75%) | 3 (16%) | 16 (84%) |
| Gynecological | 0 (0%) | 5 (100%) | 3 (50%) | 3 (50%) |
| Head and neck | 2 (100%) | 0 (0%) | 4 (57%) | 3 (43%) |
| Other | 1 (7%) | 13 (93%) | 1 (9%) | 10 (91%) |
| Benign | 0 (0%) | 4 (100%) | 0 (0%) | 2 (100%) |
| Total | 8 (15%) | 47 (85%) | 33 (33%) | 68 (67%) |
Other includes sarcoma, cutaneous, pediatric, and lymphoma.
On average, patients traveling for in-person visits had a median round trip of 44 miles (IQR, 10-98 miles). Of those patients seen via telemedicine, a median of 60 travel miles round trip was saved (IQR, 32-180 miles). Patients who attended in-person visits tended to live closer to the clinic vs those who attended via telemedicine ( P = .07). Total miles traveled for in-person visits during the 1-week period was 3842 miles; approximately 199,784 miles annually assuming the proportion of in-person to telehealth visits was representative of a typical week. For those who attended visits via telemedicine, 13,828 commuting miles were saved in 1 week and 719,056 miles annually. The forecasted annual saving of CO2e attributed to telemedicine visits was 337,829 kg, the equivalent emissions of 65.7 homes’ electricity use for 1 year.13 ( Table 3 )
Calculation Model for Greenhouse Gas Emissions Saved by Telemedicine
| GAS | HYBRID | PHEV | ELECTRIC | TOTAL | |
|---|---|---|---|---|---|
| Vehicle fleet, by vehicle type | 85% | 7% | 2% | 6% | 100% |
| Miles driven, by vehicle type | 611,198 | 50,334 | 14,381 | 43,143 | 719,056 |
| EMISSION TYPE, BY GAS | GAS | HYBRID | PHEV | ELECTRIC | TOTAL EMISSIONS, BY GAS (kg) | GWP (100y) | EMISSIONS, CO2e (kg) |
|---|---|---|---|---|---|---|---|
| VOC | 179.08 | 9.82 | .92 | 15.16 | 204.98 | Not defined | - |
| CO | 1772.47 | 138.92 | 16.39 | 6963.63 | 8891.42 | Not defined | - |
| NOx | 241.42 | 14.54 | 2.12 | .14 | 258.21 | Not defined | - |
| CH 4 | 282.98 | 16.27 | 5 | 15.16 | 319.42 | 28 | 8943.65 |
| CO 2 | 277,116.99 | 16,075.22 | 3007.02 | 6963.63 | 303,162.85 | 1 | 303,162.85 |
| NO 2 | 81.29 | 4.79 | .1 | .14 | 86.32 | 298 | 25,723.25 |
| Total emissions, CO2e (kg) | 337,829.76 |
GWPs are not defined for VOC, CO, and NOx due to short-lived atmospheric lifetime of these gases.
Abbreviations: PHEV, plug-in hybrid electric vehicle; GWP, global warming potential; CO2e, carbon dioxide equivalents.
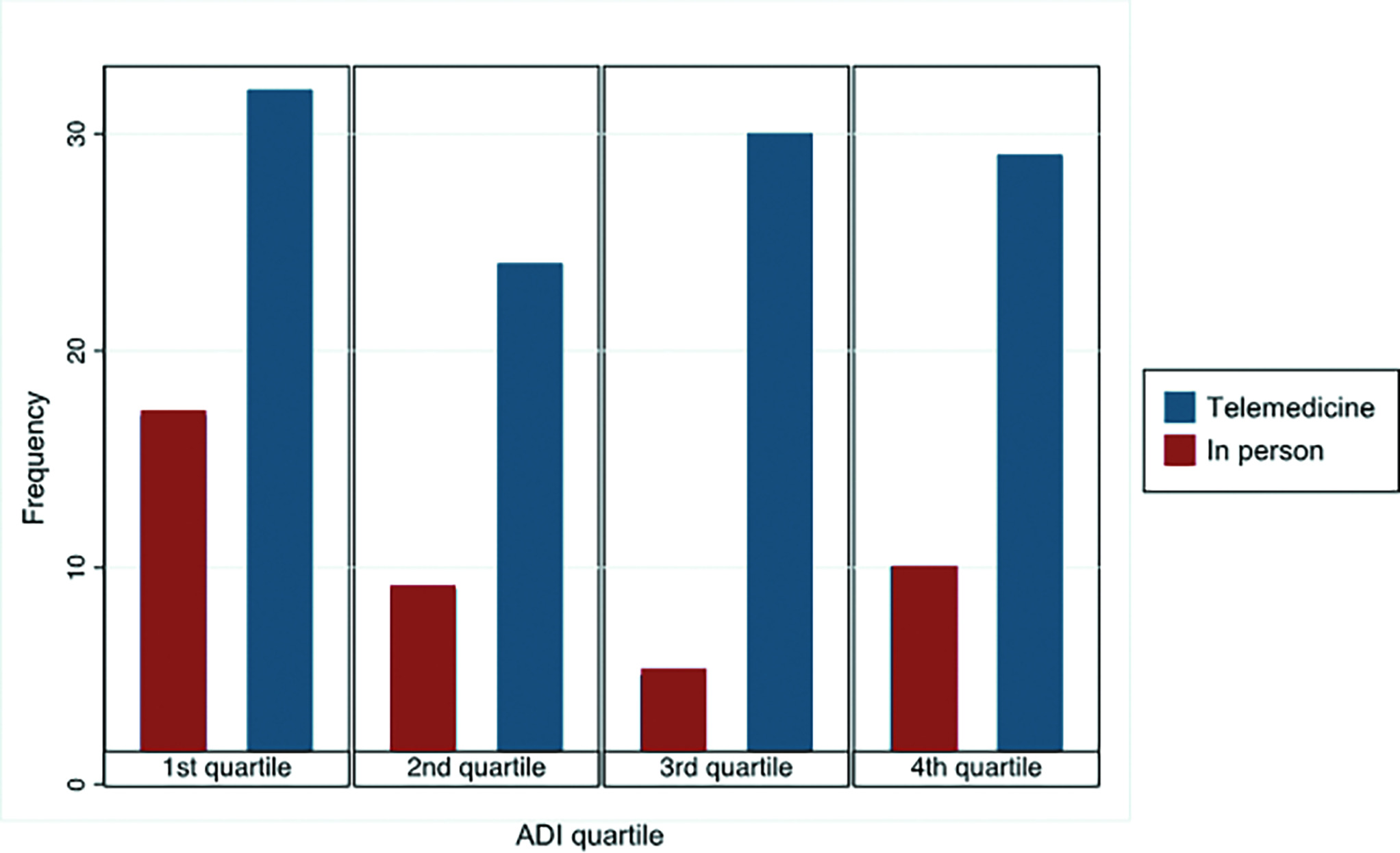
ADI, a composite measure of socioeconomic disadvantage, was not associated with the use or avoidance of telemedicine ( P = 0.22). Patients within each ADI quartile participated similarly in in-person and telemedicine visits ( Figure 1 ).
Frequency of in-person and telemedicine by Area Deprivation Index (a composite measure of socioeconomic disadvantage) quartile. A higher quartile rank represents a more disadvantaged block group.
Discussion
In this cross-sectional single-institution study, integration of telemedicine within a radiation oncology clinic resulted in a substantial reduction in carbon emissions, which when projected annually amounts to 339.8 metric tons of CO2e due to obviating the need for patient commute. In total, this translates to the equivalent emissions of 65.7 homes’ electricity use for 1 year.
When considering the environmental impact of a health care system (including a radiation therapy delivery center), one must consider both direct and indirect contributions.1 Patient transportation-associated carbon emissions account for a significant portion of health-care-associated GHG emissions and may be a large and targetable source to reduce carbon emissions.14 A case series sought to quantify the carbon footprint of the radiation therapy pathway on a per-patient basis, tallying emissions related to patient travel, energy usage of linear accelerator, energy usage of treatment planning imaging systems, treatment machine sulfur hexafluoride gas leakage, personal protective equipment, and medications required due to radiation therapy. In this series, travel represented the gross majority of a radiation oncology patient’s carbon footprint, approaching 75% to 85% of total patient-related carbon emissions and largely dominated other sources such as linear accelerator energy usage (8%-20%) (Rob Chuter, PhD, oral presentation, Christie National Health Service Foundation Trust, September 2022).
Energy usage from linear accelerator-based external-beam radiation therapy was recently estimated, and the energy required for active beam-on treatment time as well as idle time was quantified.15 The modality with the average highest carbon emissions per course was a 28-fraction course for prostate cancer, which corresponds to CO2-equivalent emissions of driving an average of 41.2 miles in a standard vehicle. Based on our data, 1 telemedicine visit saves 60 miles traveled in a standard vehicle, on average. If 1 patient converts to a telemedicine visit from in-person, the CO2-equivalent emissions saved are equal to the energy required to power almost 1.5 courses of linear-accelerator-based prostate radiation therapy. Further comprehensive assessments investigating radiation therapy patient care are needed to identify high-impact opportunities to reduce health-care-associated environmental impacts; we posit telemedicine as a potential high-impact intervention that is currently widely in use.16
There is concern that telemedicine may increase health care disparities among low-income populations given the cost associated with telemedicine visits, such as computer, internet, and/or phone service. This is particularly important as vulnerable patient groups are often at greatest risk of poor health outcomes in the face of climate change. Importantly, we demonstrate that telemedicine was used at similar rates across gender, race, ethnicity, insurance policy, and socioeconomic status, and did not differ by ADI score. We have also demonstrated that telemedicine has other positive externalities upon financial toxicities by reducing travel, time, and opportunity costs related to transportation.17 , 18 We contend that similarly climate-centered metrics should be considered when informing the choice between in-person and telemedicine visits. For telemedicine to remain accessible and equitable, continued coverage of telemedicine services by insurance payers, along with improved broadband access for rural communities under recently passed US legislation, will be critical.19 The Centers for Medicare & Medicaid Services recently announced their plan for revocation of payment parity between in-person and telehealth visits following the end of the public health emergency, during which it was required that insurers reimburse the same payment rate for telehealth services as in-person care. The exact impact on our telemedicine delivery remains to be seen; however, we can safely assume the volumes of telehealth interactions will decrease with negative impacts on health-care-related carbon emissions, health equity, and patient-facing costs.20
This piece is particularly timely, with the American Society of Radiation Oncology (ASTRO) having published its inaugural climate change policy statement earlier this year.21 In this correspondence, ASTRO recognized that climate change poses a threat to the delivery of cancer care and that these effects result in a considerable cost to patients, providers, and health care systems. They proposed key pillars for focused action against climate change that were within the scope of the society’s strategic priorities, including but not limited to (1) a need for education/engagement as well as (2) the promotion of sustainability practices. This investigation not only supports these initiatives posited by ASTRO but also should serve as an interest toward additional oncology societies who are invested in reducing their environmental footprint and increasing practice-related climate resiliency.
One of the primary barriers to standardizing telemedicine is related to patient selection and concerns that telemedicine precludes the ability of physicians to examine patients.5 Despite this, physicians report that they feel comfortable triaging whether a visit is appropriate for telemedicine or would require an in-person visit.6 The need for physical examination, or the availability of an acceptable proxy, was the primary factor for most physicians when deciding on telemedicine acceptability.7 In our experience, we found that patients whose cancer requires a physical examination (ie, nasopharyngoscopy, speculum examination) as part of disease surveillance were seen in-person at higher frequency. Patient-centered factors such as convenience, cost-effectiveness, and preference were also accepted as measures when determining telemedicine utilization. In fact, investigations specific to radiation oncology telemedicine use report high satisfaction, high utility, that most perceive equivalent or improved visit quality with telemedicine, and that a large majority would want to continue the use of telemedicine.5 - 7 Radiation oncology patients, too, demonstrate high satisfaction and confidence in their care, equivalent to in-person visits.22 Advocacy efforts should promote the use of telemedicine where appropriate in care settings to reduce financial, time, and environmental toxicity in oncology and should involve key stakeholders, including physicians and direct patient care providers, when determining payment models that could significantly limit access to this key component of oncological care delivery.
Our study has several limitations. This is a single-institution experience situated in a densely populated suburban car-centric community; therefore, the primary modality of patient commute was assumed to be by vehicle. Our department is not conveniently accessible by public transportation and few patients live close enough where foot/bike travel is feasible. Institutions in large cities may face different transportation patterns. Additionally, we did not include commutes for patients receiving daily treatment and therefore did not capture the total carbon footprint attributed to all patients commuting to our department daily. Though patient transportation-associated emissions serve as a promising opportunity to reduce the environmental impact of an oncological practice, further studies are needed to comprehensively assess the opportunity to improve care delivery while reducing emissions. The observation that patients who utilized telemedicine visits were more likely to be younger may potentially signal an age-related inability to access telemedicine and represent a barrier to care for the elderly. Finally, we recognize the limitations of extrapolating a single-week of data to yearly impact, particularly during a time of changing telehealth utilization patterns. Obtaining annual data, however, was time- and resource-prohibitive for the study, and therefore we proceeded with the acceptance that overall validity and applicability may be limited.
Conclusion
In conclusion, we demonstrate that integration of telemedicine within a radiation oncology clinic reduces the environmental impact of patient care while maintaining equitable access. Telemedicine should be considered where feasible and clinically appropriate to decrease carbon emissions associated with the practice of radiation oncology, as well as to establish and provide environmentally sustainable health care delivery in oncology.
References
Citation
Melissa A. Frick, MD, Claire C. Baniel, MD, Katie Lichter, MD, Hilary P. Bagshaw, MD. Travel-Related Environmental Impact of Telemedicine in a Radiation Oncology Clinic. Appl Radiat Oncol. 2024;(1):23 - 29.
doi:10.37549/ARO-D-23-00026
March 1, 2024