Analysis of the Radiation Oncology In-Training Examination Content Using a Clinical Care Path Conceptual Framework
Images



Abstract
Hypothesis: The American College of Radiology (ACR) Radiation Oncology In-Training Examination (TXIT) is an assess ment administered by radiation oncology training programs to assess resident performance against national benchmarks. Results are currently reported using a disease site conceptual framework. The clinical care path framework was recently proposed as a complementary view of resident education. This study assesses distribution of 2016-2019 TXIT questions using the clinical care path framework with the hypothesis that questions are unequally distributed across the clinical care path framework, leading to underassessment of fundamental clinical skills.
Methods and Materials: Using a clinical care path framework, 1,200 questions from the 2016-2019 TXITs were categorized into primary categories and subcategories. The distribution of questions was evaluated.
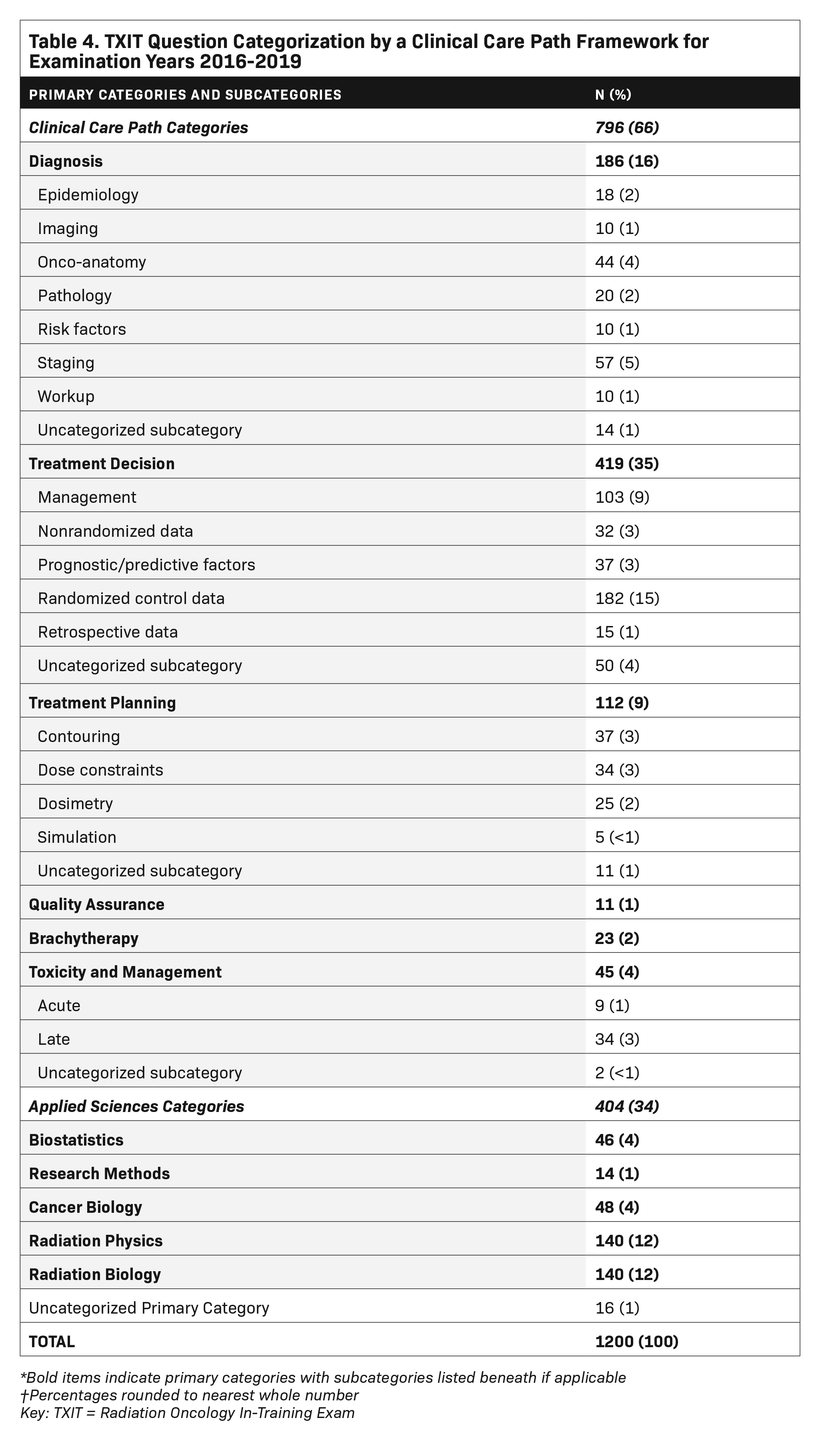
Results: Primary categorization was achieved for 98.7% of questions. Where applicable, subcategorization was achieved for 96.6% of questions. There was substantial inter-rater reliability (primary category Κ = 0.78, subcategory Κ = 0.79). Distribution of TXIT content by the clinical care path framework was: treatment decision (35%), diagnosis (16%), radiation biology (12%), radiation physics (12%), treatment planning (9%), biostatistics (4%), cancer biology (4%), toxicity and management (4%), brachytherapy (2%), quality assurance (1%), and research methods (1%). Of the 419 questions within the treatment decision primary category, knowledge from randomized clinical trials was most frequently evaluated (43%).
Conclusions: TXIT question items are unequally distributed across clinical care path categories, emphasizing treatment decision over other categories such as treatment planning and toxicity and management. Reporting examination data by both clinical care path and disease site conceptual frameworks may improve assessment of clinical competency.
The American of College of Radiology (ACR) Radiation Oncology In-Training Examination (TXIT) is a standardized assessment used to assess radiation oncology trainees’ acquisition of knowledge necessary for independent practice. By providing “mean norm-referenced scores at the national, institutional, and individual levels,” the TXIT serves as a formative assessment to inform trainees and training programs on content areas that may require additional attention for self-study or formal didactics.1-4
The annual TXIT examination consists of 300 single-answer, multiple-choice questions and is sponsored by the ACR Commission on Publications and Lifelong Learning.3 Examination content is organized into 13 sections according to a disease site conceptual framework (eg, thoracic, breast, lung), or by basic science subject (biology, physics, statistics).
In medical education, a conceptual framework facilitates organization and perception of educational content. A conceptual framework can also “represent [a] way of thinking about a problem” and influence how interrelated topics may be considered.5 Traditionally, the field of radiation oncology has used a disease site conceptual framework to organize resident education. The use of a disease site framework is reflected in didactic curricula, clinical rotations, case logs, textbooks, and board examination categories.6,7 This prevailing conceptual framework also underlies development of assessment tools such as the TXIT examination.4
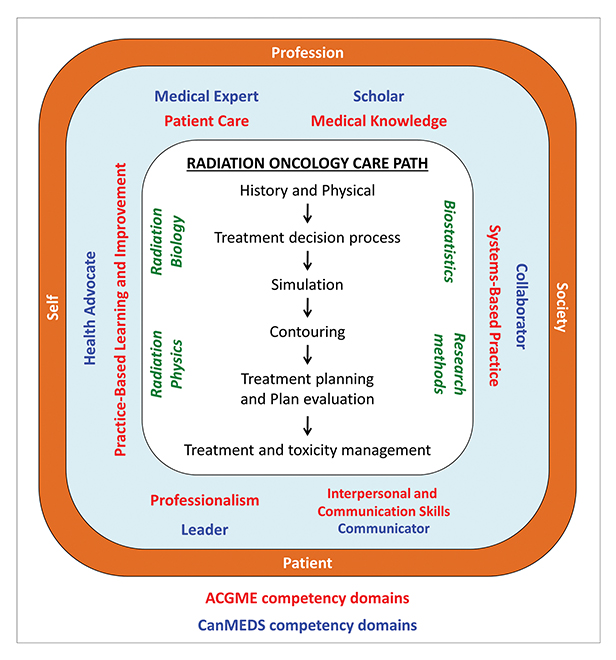
A conceptual framework based on the radiation oncology clinical care path was recently proposed and represents an alternative and complementary lens through which to view radiation oncology education (Figure 1).8 The clinical care path conceptual framework represents the stepwise clinical activities involved in providing care to a patient receiving radiation therapy. These steps begin at the initial consultation and encompass the treatment decision, simulation, contouring, treatment planning, quality assurance, toxicity management, and long-term follow-up. For medical specialties with a technical component, such a framework may better encompass the spectrum of professional activities in which a physician must demonstrate proficiency to be considered competent for independent practice. As a result, the clinical care path framework may provide a more direct link to competency-based medical education.9-11
The extent to which the TXIT assesses competency in the clinical activities central to the practice of radiation oncology as defined by the clinical care path conceptual framework is unknown. The purpose of this study was to assess the distribution of questions in the 2016-2019 TXIT examinations using the clinical care path framework. We hypothesized that the TXIT content is unequally distributed across the clinical care path framework, leading to underassessment of fundamental clinical skills.
Methods and Materials
Category Definition
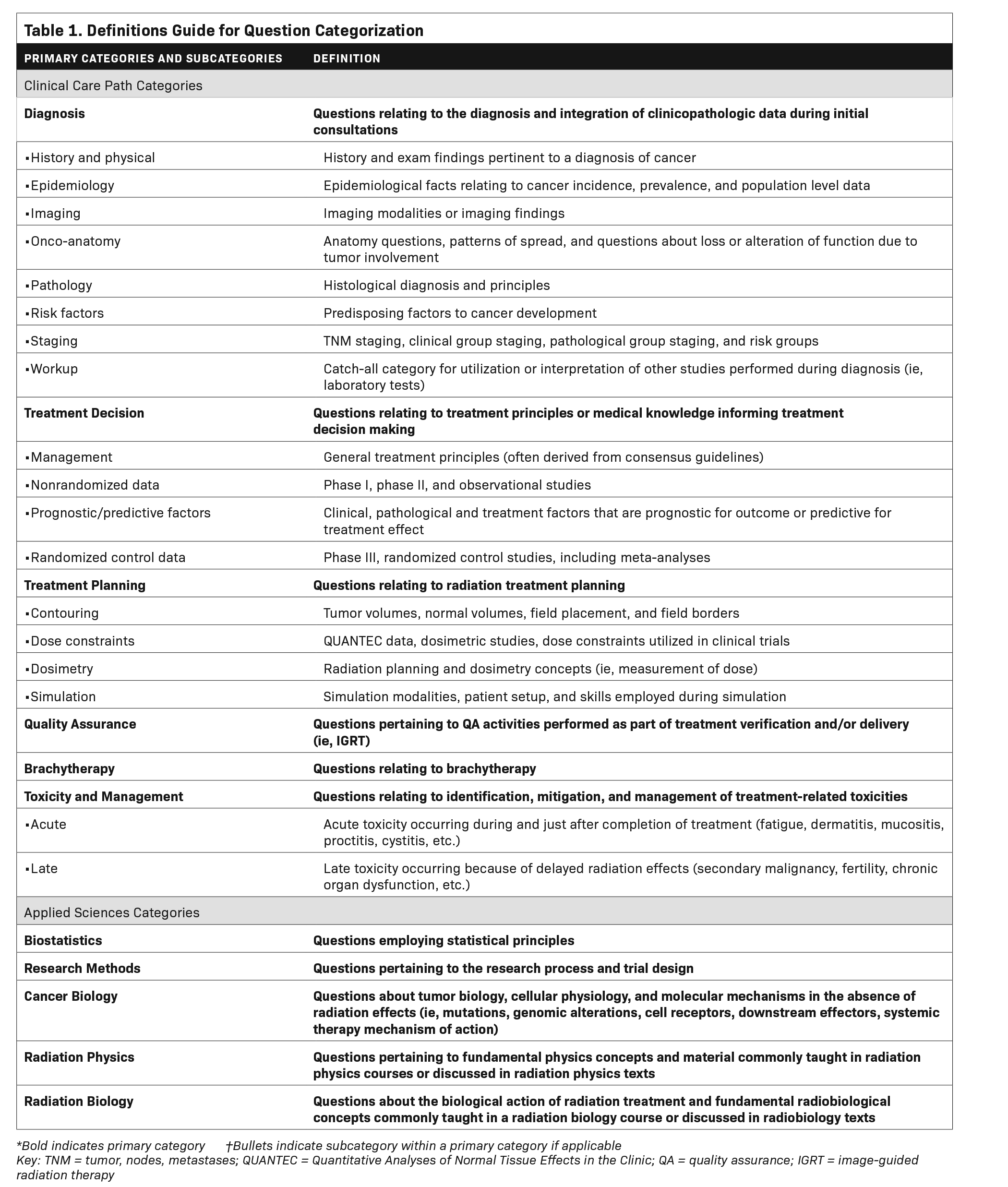
The clinical care path framework was adapted to derive clinical care path primary categories and subcategories (Figure 2) along with definitions to guide categorization by independent coders (Table 1). Subjects outside of the clinical care path but fundamental to the practice of radiation oncology including radiation biology, cancer biology, radiation physics, biostatistics, and research methods were included as separate applied sciences primary categories (Figure 2).
Coding of Question Items
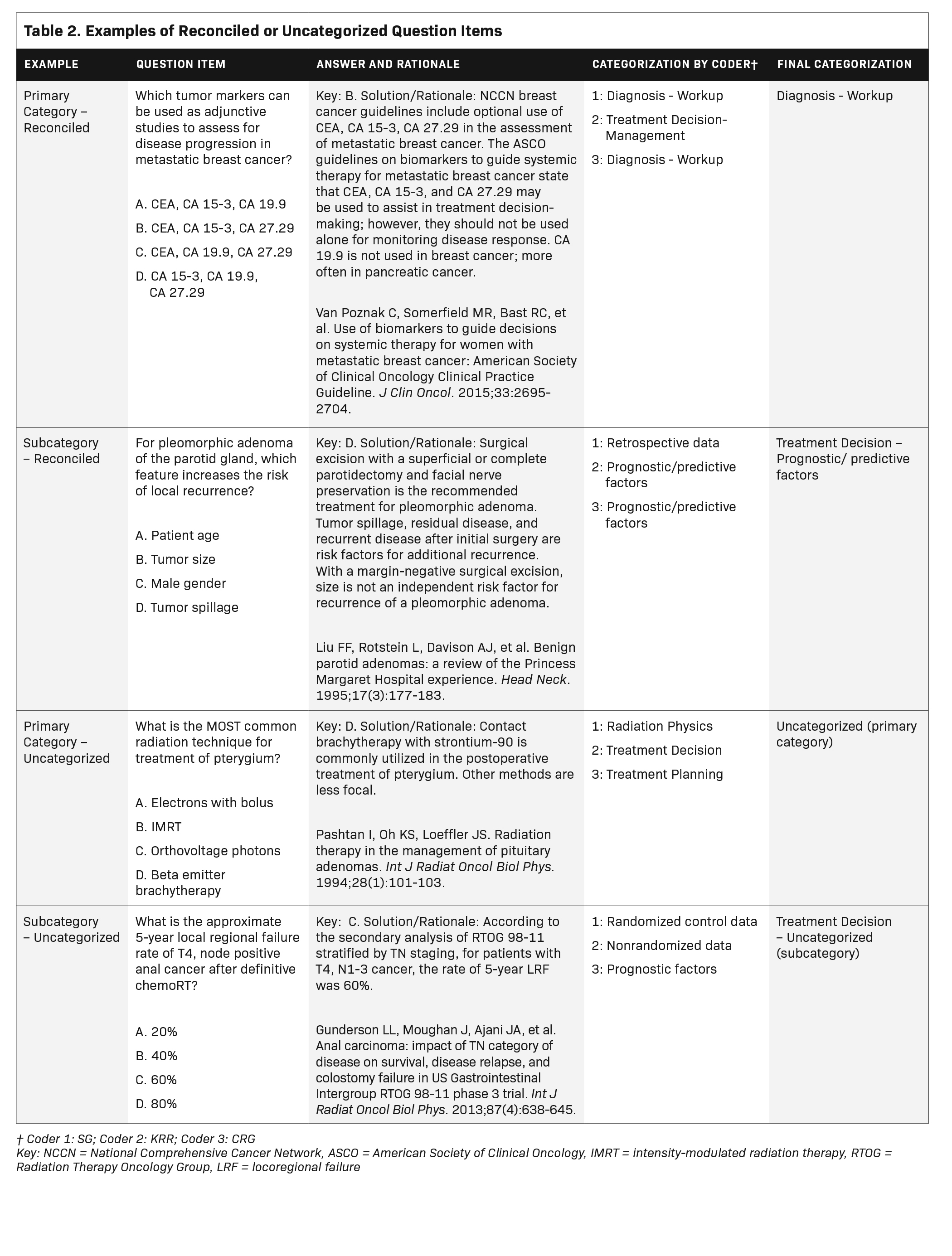
Two independent coders categorized 1,200 questions from the 2016-2019 TXIT examinations based on the content of the question stem, answer choices, and associated rationale. Inter-rater reliability was assessed with Cohen’s kappa coefficient test statistic. Items with discordant categorizations were independently reconciled by a third coder. If reconciliation was not achieved, the question was deemed uncategorizable at the primary or subcategorization level. Examples of reconciled and uncategorized questions are provided in Table 2. A single coder categorized questions according to disease site and content area. At the time of question categorization, all coders were radiation oncology residents at accredited US residency programs.
Institutional review board review of this study was not obtained as no human subjects were researched.
Results
Question Classification
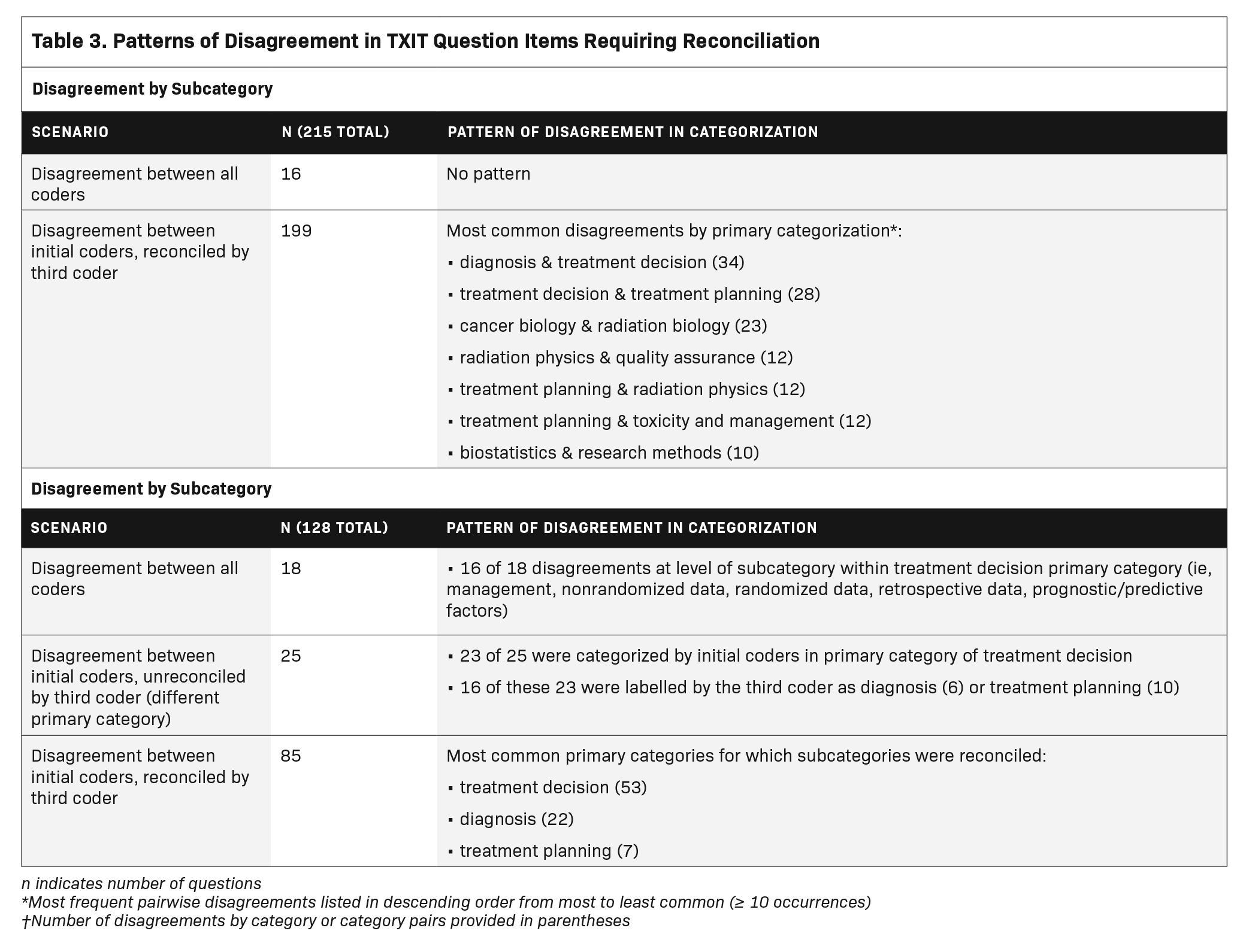
Initial question categorization was achieved with substantial agreement between two independent coders (primary category, к = 0.78; subcategory, к = 0.79). In total, 343 questions (28.6%) required categorization by a third coder. Of the 1,200 question items, 1184 (99%) were successfully categorized by primary category. Of 199 questions for which reconciliation of the primary category was achieved, items were most commonly labeled as treatment decision by one coder and either diagnosis (n = 34, 17%) or treatment planning (n = 28, 14%) by the second coder. Of the 762 question items with a subcategory, 719 (94%) were successfully subcategorized. Of 85 questions for which reconciliation of the subcategory was achieved, most were within the treatment decision (n = 55, 65%), diagnosis (n = 22, 25%), or treatment planning primary categories (n = 7, 8%). Additional details of reconciled questions are available in Table 3.
TXIT Content by the Clinical Care Path Framework
The distribution of question items from the 2016-2019 TXIT examinations according to the clinical care path framework is reported in Table 4. A total of 796 (66%) question items were classified using the clinical care path, with the remaining 404 (34%) categorized as applied sciences. Clinical care path questions assessing treatment decisions were most prevalent, representing approximately 35% of all items (n = 435). These questions most frequently evaluated data derived from randomized clinical trials (n = 182). Questions assessing diagnosis were the second most common (n = 186, 16%) and most frequently assessed tumor staging. Approximately 10% of questions assessed treatment planning (n = 112), of which approximately two-thirds were related to contouring and dose constraints. Questions evaluating treatment toxicity represented approximately 4% of items. Questions assessing brachytherapy included 23 questions within a 4-year testing period (2%).
For the applied sciences questions, radiation and cancer biology represented approximately 16% of all question items (n = 188), followed by radiation physics (n = 140, 12%), and biostatistics/research methods (n = 60, 5%).
TXIT Content by a Disease Site Framework
When classifying questions other than those defined as applied sciences according to a disease site framework, disease sites were represented approximately equally, with 6% to 8% of total questions dedicated to most sites (Table 5). Breast (n = 95, 8%) and head and neck (n = 93, 8%) were most frequently assessed, followed by lymphoma, pediatrics, genitourinary, and gynecologic disease sites (n = 73 to 83, 7%).
Discussion
Content analysis of the TXIT using a clinical care path framework demonstrates an uneven distribution in the number of questions allocated to the different steps of the clinical care path. Specifically, the exam most frequently assesses knowledge used to guide treatment decisions with fewer questions assessing treatment planning skills and management of treatment-related toxicity. This uneven distribution is not apparent when evaluating question content through a disease site framework.
In considering this uneven distribution, it is important to note that the TXIT never intended to serve as a comprehensive trainee assessment. The first chairman of the ACR Committee on Professional Testing established at the outset that “factors of clinical judgment, diagnostic skills and general sophistication in selecting a treatment program for a patient are not assessed in the in-training examination.”1 Moreover, the ACR has emphasized that the TXIT is not to be used as the principle method of assessing performance in residency, predicting success on the American Board of Radiology (ABR) written board examinations, or as a criterion for employment.5 As a result, relying on the TXIT as a measure of resident competency across all entrustable professional activities in radiation oncology is a task for which the TXIT was not designed.
Underassessment of certain competencies may be inherent to written examinations in medical education, as evidenced by content analysis of the plastic surgery and orthopedic surgery in-training examinations, which showed unequal distributions of in-training exam content relative to the Accreditation Council for Graduate Medical Education (ACGME) Milestones and competencies.12 In particular, there appears to be a bias for test-makers with regard to the type of questions included on written in-training examinations with respect to available published evidence on which those questions are based. A content analysis of the plastic surgery in-training examination found there were significantly more Level III (decision-making questions) compared to Level I (fact recall) or Level II (interpretation questions). In addition, Level III questions more frequently justified the correct answer by referencing a journal article, with an overall higher mean number of journal references cited for these questions compared with other question types.13 One possible explanation for this finding is that decision-making questions may be easier to develop because consensus exists due to the availability of supporting data.
When extrapolating this to the TXIT exam, and our own finding that treatment decision questions are predominant, we hypothesize there may be fewer questions from underrepresented clinical care path categories because there are fewer data on which to base single best answers. In other words, an acceptable range of choices exists. As an example, the preferred method to position a patient for set-up during computed tomography (CT) simulation may vary among radiation oncologists. Multiple set-up positions may be considered correct, so developing a multiple-choice question to assess a trainee’s CT simulation knowledge may be challenging. Our analysis of the TXIT exam content is unable to support or refute this hypothesis as an explanation for the bias toward treatment decision questions. To remedy this, exam item writers may benefit from training on how to develop a multiple-choice question assessing knowledge that is not based on journal publications, but that is required to function as a competent radiation oncologist.
Nevertheless, the TXIT continues to serve a singular and influential role in formative assessment of radiation oncology trainees as it is the only assessment tool that allows residency programs to benchmark their trainees against national metrics. Acknowledging the prominence of the TXIT in resident assessment, residency programs should encourage realignment of the exam to better assess underrepresented radiation oncology clinical care path competencies. Although changes to the TXIT as suggested in Table 6 may accomplish this goal, the effort and resources required to do so may be prohibitive.
Alternatively, instead of retrofitting the TXIT to improve assessment of specific competencies, a better strategy may be to develop new assessment methods that target specific components of the radiation oncology clinical care path in which trainees are underassessed. For example, residents in the US and Canada have identified a general absence of formal instruction and assessment in treatment planning that impedes transition to independent clinical practice.14-16 To address this curricular deficiency, radiation oncology educators could make a concerted effort to create teaching resources and assessment tools to promote and measure acquisition of treatment planning skills. Potential advantages of this approach include removing constraints imposed by a multiple-choice format, incorporating performance-based assessment, and using multiple assessment tools to triangulate trainee competency.17,18
Finally, it would be of interest to analyze the ABR Clinical Radiation Oncology Qualifying Exam according to the radiation oncology clinical care path framework. If current formative and summative assessments in the US do not assess for clinical competency across the entire clinical care path, then practicing clinicians may be deficient in specific areas. Further inquiry is needed into the development of comprehensive assessment methods to ensure clinical competency across the clinical care path.
This study has several limitations. First, the categorization of questions is inherently subjective despite utilizing multiple coders to avoid incorrect or inconsistent categorization. Among questions in which the initial two coders disagreed there was frequent overlap between the diagnosis, treatment decision, and treatment planning categories. This likely stems from the abundance of treatment decision questions and the inherent overlap of content with adjacent clinical care path primary categories of diagnosis and treatment planning. The small number of quality assurance questions may be due to significant overlap with the radiation physics category, making it difficult to conclude whether this is an underrepresented content area based on our analysis. Furthermore, the level of agreement between initial categorization by two coders is only moderate and not all question items were categorized through our reconciliatory process. These findings suggest there are other conceptualizations of a clinical care path framework that may improve categorization and better facilitate analysis of exam content.
Conclusions
Radiation oncology ACR TXIT questions are unequally distributed along the radiation oncology clinical care path conceptual framework. The exam contains a higher proportion of questions pertaining to treatment decisions than questions assessing other clinical skills such as treatment planning, toxicity management, and brachytherapy. To the extent that the TXIT reflects national licensing exams and, more broadly, content prioritized in radiation oncology education, deficiencies in education and assessment within specific areas of the radiation oncology clinical care path may manifest as deficiencies in clinical competency among radiation oncology trainees. Acknowledging there is no singular assessment that can holistically measure trainees’ preparedness for independent practice, radiation oncologists in training and their future patients would benefit from additional assessment tools to comprehensively assess knowledge and skills fundamental to all aspects of the practice of radiation oncology.
References
- Wilson JF, Diamond JJ. Summary results of the ACR (American College of Radiology) experience with an in-training examination for residents in radiation oncology. Int J Radiat Oncol Biol Phys. 1988;15(5):1219-1221. doi:10.1016/0360-3016(88)90207-6
- Coia LR, Wilson JF, Bresch JP, Diamond JJ. Results of the in-training examination of the American College of Radiology for Residents in Radiation Oncology. Int J Radiat Oncol Biol Phys. 1992;24(5):903-905. doi:10.1016/0360-3016(92)90472-t
- DXITTM and TXITTM In-Training Exams. Accessed January 20, 2020. https://www.acr.org/Lifelong-Learning-and-CME/Learning-Activities/In-Training-Exams. Published 2020.
- Hatch SS, Vapiwala N, Rosenthal SA, et al. Radiation Oncology Resident In-Training examination. Int J Radiat Oncol Biol Phys. 2015;92(3):532-535. doi:10.1016/j.ijrobp.2015.02.038
- Bordage G. Conceptual frameworks to illuminate and magnify. Med Educ. 2009;43(4):312-319. doi:10.1111/j.1365-2923.2009.03295.x
- Accreditation Council for Graduate Medical Education (ACGME). ACGME Program Requirements for Graduate Medical Education in Radiation Oncology; 2020. Accessed January 2021. https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/430_RadiationOncology_2020.pdf?ver=2020-02-20-135340-140
- American Board of Radiology Study Guide for Clinical (General and Radiation Oncology). Accessed July 1, 2020. https://www.theabr.org/radiation-oncology/initial-certifica
- tion/the-qualifying-exam/studying-for-the-exam/clinical-radiation-oncology. Published 2020.
- Golden DW, Ingledew P-A. Radiation Oncology Education. In: Perez and Bradys Principles and Practice of Radiation Oncology. 7th ed. Lippincott, Williams & Wilkins; 2018:2220-2252.
- Accreditation Council for Graduate Medical Education (ACGME). Common Program Requirements (Residency). 2020:1-55. Accessed July 1, 2020. https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/CPRResidency2020.pdf
- The radiation oncology milestone project. J Grad Med Educ. 2014;6(1s1):307-316. doi:10.4300/jgme-06-01s1-27
- Carraccio C, Englander R, Van Melle E, et al. Advancing competency-based medical education: a charter for clinician-educators. Acad Med. 2016;91(5):645-649. doi:10.1097/ACM.0000000000001048
- Ganesh Kumar N, Benvenuti MA, Drolet BC. Aligning in-service training examinations in plastic surgery and orthopaedic surgery with competency-based education. J Grad Med Educ. 2017;9(5):650-653. doi:10.4300/JGME-D-17-00116.1
- Silvestre J, Bilici N, Serletti JM, Chang B. Low levels of evidence on the plastic surgery in-service training exam. Plast Reconstr Surg. 2016;137(6):1943-1948. doi:10.1097/PRS.0000000000002164
- Moideen N, de Metz C, Kalyvas M, Soleas E, Egan R, Dalgarno N. Aligning requirements of training and assessment in radiation treatment planning in the era of competency-based medical education. Int J Radiat Oncol Biol Phys. 2020;106(1):32-36. doi:10.1016/j.ijrobp.2019.10.005
- Best LR, Sengupta A, Murphy RJL, et al. Transition to practice in radiation oncology: mind the gap. Radiother Oncol J Eur Soc Ther Radiol Oncol. 2019;138:126-131. doi:10.1016/j.radonc.2019.06.012
- Wu SY, Sath C, Schuster JM, et al. Targeted needs assessment of treatment planning education for united states radiation oncology residents. Int J Radiat Oncol Biol Phys. 2020;106(4):677-682. doi:10.1016/j.ijrobp.2019.11.023
- Van Der Vleuten CPM, Schuwirth LWT, Driessen EW, et al. A model for programmatic assessment fit for purpose. Med Teach. 2012;34(3):205-214. doi:10.3109/0142159X.2012.652239
- Miller GE. The assessment of clinical skills/competence/performance. Acad Med. 1990;65(9 Suppl):S63-7. doi:10.1097/00001888-199009000-00045
Citation
Rogacki KR, Gutiontov S, Goodman CR, Jeans E, Hasan Y, Golden DW. Analysis of the Radiation Oncology In-Training Examination Content Using a Clinical Care Path Conceptual Framework. Appl Radiat Oncol. 2021;(3):41-51.
October 5, 2021
