Asymptomatic pneumomediastinum, subcutaneous cervical emphysema without esophageal tear following pneumoperitoneum
Images


CASE SUMMARY
More than 500 000 cases of head and neck cancer are diagnosed worldwide each year.1 Placement of a gastrostomy tube (G-tube) is often needed during definitive radiation therapy (+/- chemotherapy) for cancers of the head and neck. Although this procedure is usually uncomplicated, it is reportedly associated with a complication rate of 13.7% and mortality rate of 0.3%.2 Pneumoperitoneum is common after such procedures, and is self-limited when no findings indicate organ perforation.3 Pneumomediastinum, on the other hand, is a rare complication after G-tube placement.4 In general, pneumomediastinum may occur due to a complete tear of the esophagus (secondary to direct trauma or violent vomiting with retching), spontaneous pneumothorax, or gangrenous (gas-forming) infections.5,6 We present a rare case of a patient who was incidentally found to have asymptomatic pneumomediastinum and subcutaneous emphysema of the neck approximately two weeks after G-tube placement without evidence of an esophageal tear.
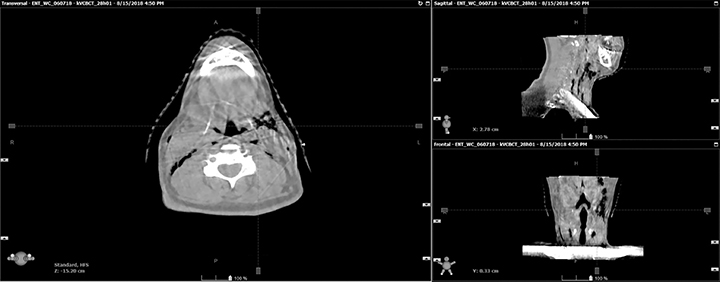
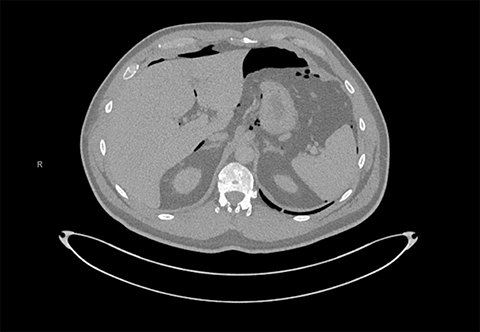
A 48-year-old man was diagnosed with p16 positive squamous cell carcinoma of the base of the tongue with bilateral cervical lymphadenopathy (stage II, cT2N2M0, American Joint Committee on Cancer [AJCC] 8th edition). He was treated definitively with intensity-modulated radiation therapy (IMRT) with concurrent weekly cisplatin 40 mg/m2. Reactive placement of a gastrostomy tube became necessary when oral intake decreased substantially. This tube placement was advised prophylactically but at the outset was refused. The patient had a violent gag reflex initially, rendering routine oral examination difficult. Starting on day 2 of radiation therapy and chemotherapy, he developed vomiting that became intractable. On day 28 of the radiation therapy course after 34 Gy / 17 fractions over 23 days, percutaneous endoscopic gastrostomy (PEG) tube placement was attempted but failed due to an inability to find a clear window with transillumination. The patient subsequently underwent G-tube placement under fluoroscopic guidance by the interventional radiologist and was discharged in stable condition. Over the following two weeks of treatment, he continued to experience persistent nausea, vomiting, and retching despite the use of various anti-emetics and benzodiazepines (prescribed for extreme anxiety). At fraction #27 of radiation therapy, daily cone-beam computed tomography (CBCT) that was obtained as part of intensity-guided radiation therapy (IGRT) showed subcutaneous emphysema (Figure 1) not present on prior imaging. At the time, the patient had no chest pain, dyspnea or fever, and there was no evidence of respiratory or hemodynamic instability. On examination, the chest and precordium were unremarkable, vital signs were normal, and a crepitus of subcutaneous emphysema could be elicited in the left side of the neck from the left angle of the mandible down to the supraclavicular region. A CT of neck/chest/abdomen with IV contrast revealed pneumoperitoneum (Figure 2), pneumomediastinum (Figure 3), and subcutaneous emphysema in the neck (Figure 4). An oral Gastrografin (Bracco Diagnostics Inc., Monroe Township, New Jersey) study was attempted but his odynophagia and retching rendered it impossible to perform. An esophagogastroduodenoscopy (EGD) was carefully performed with caution (minimizing air insufflation). There was no esophageal tear and the esophageal mucosa appeared entirely normal with no evidence of mucositis. A fluoroscopic upper GI series with small bowel follow-through was obtained by introducing Gastrografin through the G-tube and did not show extraluminal contrast extravasation. He was observed as an inpatient for one week and remained hemodynamically stable and free of clinical evidence of mediastinitis or respiratory distress. Follow-up imaging revealed resolving pneumoperitoneum, pneumomediastinum, and subcutaneous emphysema. The patient was discharged in stable condition and completed his radiation therapy course. At the end of his course, the cervical lymphadenopathy could no longer be palpated and no tumor could be seen at the primary site on examination.
IMAGING FINDINGS AND DISCUSSION
We report on a patient who was incidentally noted to have pneumomediastinum, and subcutaneous neck emphysema approximately two weeks after G-tube placement without attributable symptoms and without evidence of esophageal tears. Yount et al described two patients who developed symptomatic pneumomediastinum without esophageal perforation within 24 hours after PEG.4 To our knowledge there have been no reports of pneumomediastinum development and subcutaneous emphysema after pneumoperitoneum following G-tube placement with no mediastinal symptoms.
Pneumomediastinum is most concerning for esophageal perforation, particularly in patients with a history of vomiting and retching as was the case with our patient. Patients usually present with retrosternal chest pain, dyspnea, cough, esophageal odynophagia, or dysphagia, and quickly deteriorate into hemodynamic shock.7 A high level of suspicion is warranted as delayed diagnosis can have a significant prognostic impact with mortality ranging from 20% to 35%.8 Gastrografin esophagram remains the standard for diagnosing esophageal rupture but may have a false negative rate of up to 10%. Endoscopy is controversial as the endoscope together with the insufflated air may enlarge a perforation and worsen the condition. Treatment of pneumomediastinum may involve surgery or nonoperative management, including nothing by mouth for 24-48 hours, broad spectrum antibiotics for 7-10 days, and total parenteral nutrition.9
In our patient, esophageal rupture was ruled out by endoscopy and the source of air may be explained by two potential processes: First, pneumoperitoneum, a fairly common complication of G-tube placement, with an incidence as high as 50% following such procedures, may be a potential source of air tracking back to the mediastinum. The source of pneumoperitoneum, in turn, may be insufficient fixation of the tube into the peritoneal cavity. Alternatively, air may escape into the peritoneal cavity during the procedure when the needle punctures the abdominal wall and stomach.10 In most cases, pneumoperitoneum following PEG is a benign and self-limited process that does not require additional intervention.3
In most patients there is no direct path for air to escape from the peritoneum to the mediastinum, but pneumoperitoneum may result in pneumomediastinum via the diaphragmatic hiatus as a result of congenital anomalies, weak points, defects, or tears near the diaphragmatic hiatus.11-12 The risk of developing pneumomediastinum in this manner is thought to be associated with high intraperitoneal pressures, which was likely the case in our patient who was persistently retching. From the mediastinum, air can potentially dissect the fascial planes, which ultimately manifests as subcutaneous emphysema in the neck.
An alternative mechanism to explain the pathogenesis of pneumomediastinum in our patient is the development of a “spontaneous pneumomediastinum” as originally described by Louis Hamman in 1939. Caceres et al found Valsalva maneuvers, particularly emesis, and sudden increase of intrathoracic pressure to be the predominant initiation event of spontaneous pneumomediastinum in their retrospective review.13 In much the same manner as above, air may enter directly into the abdominal cavity through a pleuroperitoneal defect.12
Regardless of the source of air, this patient’s pneumomediastinum was incidentally noted on daily CBCT, which is otherwise utilized to verify patient alignment.14 This case highlights the importance of using daily imaging not only for geometric verification purposes, but also for evaluating anatomical changes that may warrant additional workup or a pause in treatment. Moreover, the patient’s pneumomediastinum proved to be clinically inconsequential and slowly resolved spontaneously. Despite the absence of sequelae from this process, one must maintain a high level of concern with this radiographic finding as any delay in diagnosis of a possible underlying esophageal tear may result in significant morbidity and mortality. Further studies are warranted to determine the incidence and implications of this rare finding during the treatment of head and neck cancer patients who require G-tube insertion.
CONCLUSIONS
We report on an interesting and rare finding of pneumomediastinum and subcutaneous emphysema of the neck approximately two weeks after G-tube placement incidentally detected on CBCT. The value of the case report is to call attention to identifying this rare problem, to emphasize that in this case it was not associated with a poor outcome contrary to the usual expectation with pneumomediastinum, and to report an additional advantage of frequent CBCT.
REFERENCES
- Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136(5):E359-386.
- Wollman B, D’agostino HB, Walus-wigle JR, Easter DW, Beale A. Radiologic, endoscopic, and surgical gastrostomy: an institutional evaluation and meta-analysis of the literature. Radiology. 1995;197(3):699-704.
- Wiesen AJ, Sideridis K, Fernandes A, et al. True incidence and clinical significance of pneumoperitoneum after PEG placement: a prospective study. Gastrointest Endosc. 2006;64(6):886-889.
- Yount KW, Mallory MA, Turza KC, Griffiths ER, Lau CL, Sawyer RG. Pneumomediastinum after percutaneous endoscopic gastrostomy tube placement: report of two cases. Ann Thorac Surg. 97.2 (2014): e37-e39.
- Newcomb AE, Clarke CP. Spontaneous pneumomediastinum: a benign curiosity or a significant problem? Chest. 2005;128(5):3298-3302.
- Maunder RJ, Pierson DJ, Hudson LD. Subcutaneous and mediastinal emphysema: pathophysiology, diagnosis, and management. Arch Intern Med. 1984;144(7):1447-1453.
- Brauer RB, Liebermann-meffert D, Stein HJ, Bartels H, Siewert JR. Boerhaave’s syndrome: analysis of the literature and report of 18 new cases. Dis Esophagus. 1997;10(1):64-68.
- Larsen K, Skov jensen B, Axelsen F. Perforation and rupture of the esophagus. Scand J Thorac Cardiovasc Surg. 1983;17(3):311-316.
- Brinster CJ, Singhal S, Lee L, Marshall MB, Kaiser LR, Kucharczuk JC. Evolving options in the management of esophageal perforation. Ann Thorac Surg. 2004;77(4):1475-1483.
- Iscan Y, Karip B, Ozcabi Y, Ağca B, Alahdab Y, Memisoglu K. Pneumoperitoneum with subcutaneous emphysema after percutaneous endoscopic gastrostomy. Case Rep Surg. 2014;2014:726878.
- Cunningham, AJ. Laparoscopic surgery—anesthetic implications. Surg Endoscop. 1994;8(11):1272-1284.
- Hillman KM. Pneumoperitoneum—a review. Crit Care Med. 1982;10(7):476-481.
- Caceres M, Ali SZ, Braud R, Weiman D, Garrett HE. Spontaneous pneumomediastinum: a comparative study and review of the literature. Ann Thorac Surg. 2008;86(3):962-966.
- Gupta T, Narayan CA. Image-guided radiation therapy: physician’s perspectives. J Med Phys. 2012;37(4):174-182.
Citation
Patel NV, Elsayyad N, Sidani C. Asymptomatic pneumomediastinum, subcutaneous cervical emphysema without esophageal tear following pneumoperitoneum. Appl Radiat Oncol. 2019;(2):54-56.
July 11, 2019
