Personalizing Approaches to Patient Education Throughout the Radiation Oncology Workflow
Images
Abstract
For cancer patients who undergo radiation therapy (RT) at some part of their treatment journey, new knowledge regarding the principles underlying RT, workflow, and side effects can become overwhelming and lead to patient fear and anxiety. Various patient education tools have been implemented in radiation oncology clinics internationally including virtual reality, educational videos, educational sessions, websites, and pamphlets.
Although studies have demonstrated that such tools can increase patient knowledge regarding RT and its side effects while also decreasing patient anxiety, it is unclear how best to personalize each patient’s education.
Similarly, patient characteristics such as age, gender, literacy level, and cultural considerations can also impact a patient’s need or desire for specific educational tools. Barriers to optimization include cost and resource availability with virtual reality, online misinformation, and pamphlets that may be written at an educational level higher than the average population reading level. The efficacy of different educational methods has been studied at various time points throughout the radiation oncology workflow. Overall, early educational intervention with continued reinforcement throughout the treatment course through an individualized multimodal learning approach is likely to be most effective.
Keywords: patient education, direct patient care, medical physicists, virtual reality
Approximately half of patients diagnosed with cancer will receive radiation therapy (RT) as part of their treatment course.1 Receiving a cancer diagnosis can instill fear and anxiety in patients, particularly regarding the uncertainty of what to expect during treatment.
Specific to RT, most patients and caregivers do not possess a sound understanding of treatment and often present with misconceptions about its effects, such as treatment-induced radioactivity.2 Providing effective education to patients upon consultation is challenging. Up to 30% of words used during an initial RT consultation can be identified as medical jargon, potentially compromising knowledge retention following an RT consultation.3,4 This can be problematic for patients emotionally, and can disrupt the consent process and treatment compliance.5 Providing education on RT terminology, logistics, and workflow plays an important role in achieving successful treatment outcomes. Patients who receive education show higher levels of understanding and lower levels of anxiety surrounding their radiation treatment.6-9
Although supplementary educational materials are valuable, they should not replace interactions and relationships between patients and health care providers during which patients’ unique needs and learning styles can be individualized. Demographic characteristics including male gender and older age have been associated with lower requests for information during RT consultation.10 As this suggests, there is no one-size-fits-all approach to patient education within radiation oncology; rather, each patient has different educational needs depending on age, gender, and educational level. Similarly, cultural differences including language may be a barrier to providing patients with generalized information. Radiation oncologists and allied health care staff should consider implementing individualized patient-centered educational tools into the clinical workflow to enhance patients’ understanding of their radiation treatment. The purpose of the current PubMed literature review is to present an overview of multiple educational modalities within radiation oncology patient education, their costs and benefits, where each technology may be best utilized within the RT treatment course, and how to adapt different tools to personalize the educational experience.
Patient Education Methods
Virtual Reality
Virtual reality (VR) is a more recently instituted technology for educating patients about RT. One example of its use is Virtual Environment for Radiotherapy Training (VERT).5,11 VERT is displayed via a projection screen and serves to create an interactive 3-dimensional (3D) RT treatment room environment consisting of clinical tools such as a linear accelerator, patient couch, and radiation fields.5 RT treatment plans in Digital Imaging and Communication in Medicine (DICOM) can be uploaded to display patient-specific anatomy, doses, tumor and target volumes, and therapy techniques.11 Additional studies have used VR headsets and 360-degree video tours to show patients a virtual version of themselves undergoing RT.9,12
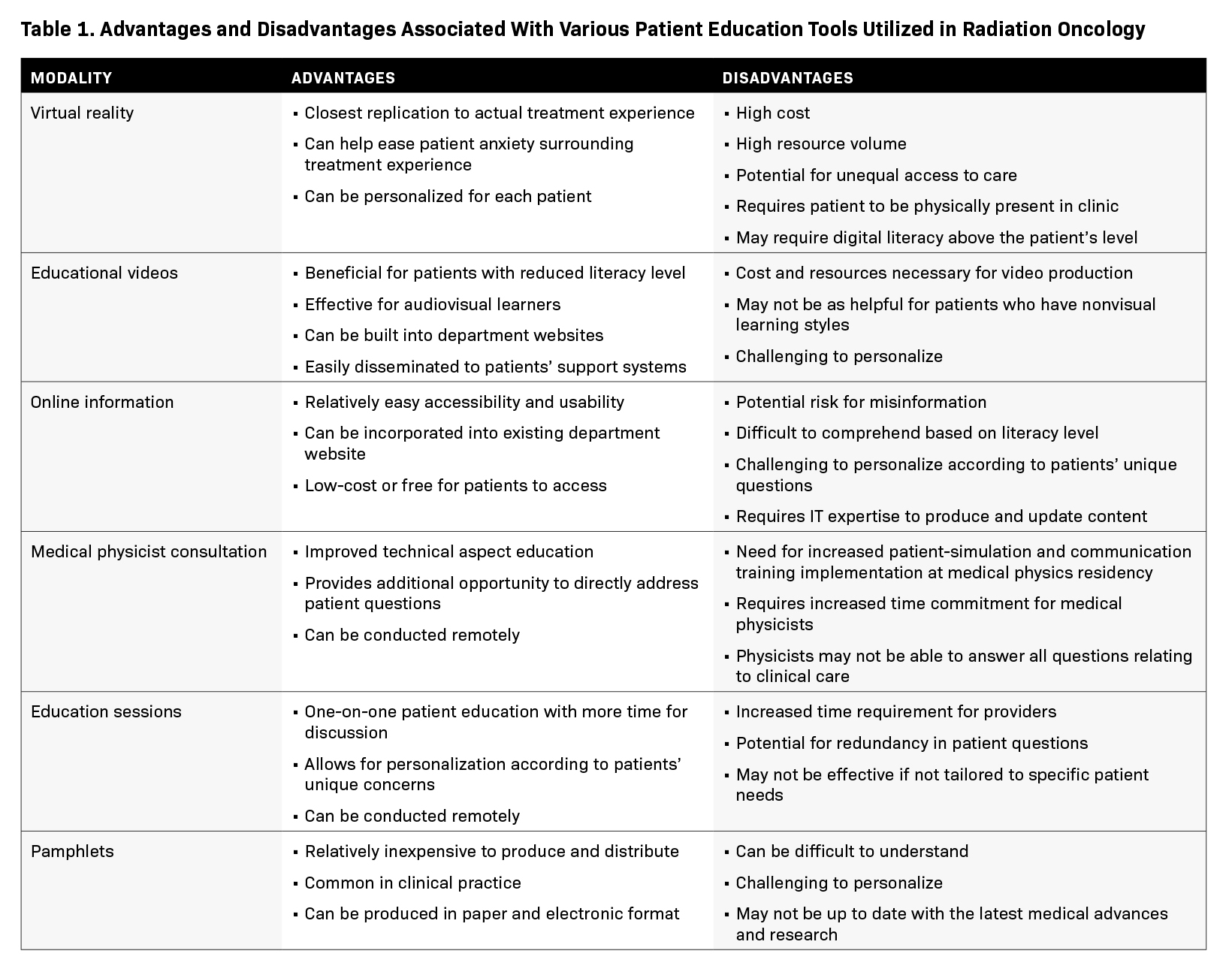
Overall, studies have demonstrated that VERT provides a basis for treatment expectations and therapy precision.5 VERT has also lowered patient anxiety, likely by enabling patients to directly envision the clinical experience in a nonclinical environment.13 The 3D environment creates a bridge that closes the gap between written educational materials and the treatment experience. This form of learning may be well-suited for patients who are visuospatial learners and those who prefer interactive learning. However, virtual reality is not without its challenges. For example, displaying DICOM images with treatment parameters may unnecessarily overwhelm and distress patients.5 Logistically, VERT requires a high volume of resources upfront that may rely on institutional budgets, leading to inequality in access to care.5
Educational Video
Verbal communication regarding the RT process, including discussion of face masks and equipment, can increase fear during a patient’s consultation.6 By visually describing the RT workflow, educational videos provide a realistic image of what to expect during treatment. Videos are advantageous because patients can view them prior to a consultation, reducing time on basic explanation and increasing time for specific patient questions during an appointment.14 Videos can also be effective for a wider variety of patient populations, including audiovisual learners or those with reduced literary skill. Additionally, patients can watch educational videos multiple times for longitudinal reinforcement. Given the significant logistical barriers to undergoing a lengthy radiation treatment process, many patients rely on their support network while undergoing RT. Another benefit of educational videos is that patients can easily share them with family and friends, improving understanding of the treatment process.
Studies have demonstrated an increase in patient knowledge of RT side effects and workflow after watching an approximately 20-minute educational video, demonstrating its value as a tool to educate a diverse patient population.2,6,15 Although online and video-based education can be a powerful tool, some patients may have limited ability to benefit from these modalities due to limited technological literacy or access. Those without reliable access to technology or who lack the basic skills to navigate online video platforms may have difficulty taking full advantage of online and video-based education. Those not comfortable using technology may be overwhelmed by video-based education, making learning more difficult.
Online Information
Due to the general lack of knowledge surrounding RT, patients and caregivers may search the internet to learn more about their treatment, leading them to departmental websites and social media outlets such as YouTube, Twitter, and TikTok.6
A major benefit to these sites as educational tools is the increasing internet accessibility and flexibility of use. Some patients may read web-based content before their initial RT appointment to help guide expectations and foster understanding of treatment options prior to physician recommendations.16 This can lead to thoughtful discussion and help build a patient-physician relationship, but could also lead to misinformation, especially since it is difficult to discern accurate from inaccurate information online.17 Misinformation online can generate negative consequences, such as patients believing they will emit radiation to loved ones after treatment or viewing their disease as an impending death.17 With increased patient anxiety, health care providers are forced to spend more appointment time counteracting and refuting misinformation read online.17
An analysis of academic radiation oncology department websites demonstrated that website language reached far above the reading level of an average adult, or the seventh to ninth grade reading level.16 Similarly, information presented on academic departmental websites may be intended for physicians, residents, medical students, or others who might have an advanced baseline knowledge of the associated medical topic.16 The National Assessment of Adult Literacy study demonstrated that most US adults lack the health literacy to understand most information provided through different educational modalities.18
Although most studies analyzing online health care language readability involve the English language, more recent studies have compared online English and Spanish content.19,20 One study comparing online pancreatic cancer treatment information found that English content was written at a university level while Spanish content was written at a high school level.19 Both English and Spanish content exceeded the average reading level for an adult.19,21 These findings suggest that readability issues with online materials span across languages and cultures.19 It is imperative that educational materials such as academic websites should aim to best align to the literacy level and the language/linguistic needs of the general population, to ensure patients are appropriately informed in their search for RT educational content. Strategies to reduce the challenge of readability of online information include incorporating less complex language and acronyms, shortening sentences, and providing links to audiovisual material.20
Medical Physicist Clinical Role
As technical experts, medical physicists play an integral role in treatment planning and patient quality assurance measurements. Their educational training and expertise facilitate patient discussions of technical details of radiation treatment (eg, type of radiation, dose, and delivery method). Confusion and concerns about complex imaging and treatment modalities often arise. Clinical trials have suggested that medical physicists, with their relevant training and knowledge, have potential to fill the gap on technology education.22,23
Studies reviewing one-on-one physicist-patient consults have demonstrated a unique avenue for patient education and anxiety reduc- tion.22,23 In studies where the intervention-arm patients met with a medical physicist, the patients were surveyed for anxiety and distress levels.22,24 The medical physicists addressed technical aspects and questions at multiple points of treatment (eg, at treatment simulation, before the first treatment, and before completion). Anxiety was significantly reduced in patients who met with a medical physicist throughout treatment, demonstrating a unique and beneficial role of physicist-patient consults.22,24 Furthermore, the consults also enabled patients to develop a more robust understanding of what to expect during treatment.25
Education Sessions
Preparing patients for RT includes addressing their complex emotions and distress. Educational sessions specifically aimed at minimizing psychological distress while expanding patient understanding have shown to be effective in a number of studies.26 Both one-on-one video conferencing and face-to-face individualized consultations have demonstrated increased patient satisfaction.27,28 Although the additional intervention varied along the RT workflow in these studies, the educational framework incorporated individualized written and verbal information at additional education-focused appointments. This material was presented by multiple members of the interdisciplinary team, including nurses, radiation therapists, physicists, and physicians, each bringing unique perspectives to the patient. Along with time for additional questions, information included general RT materials, side effects and management, and anticipated stressors.27-29
Education sessions significantly reduced in anxiety scores in patients who received 2 consultations with a radiation therapist prior to planning and treatment in addition to decreased depression scores in patients receiving a teaching session by a clinical nurse.27,29 Video conferencing with visual tele-education materials prior to simulation also demonstrated high patient satisfaction with preparation and education.28
Providers should take special considerations when conducting education sessions with patients whose primary language is one other than English, using certified medical interpreters. In-person interpretation may offer greater personalization during the treatment visit as opposed to phone interpretation, although availability may be limited throughout the entire treatment workflow.30 Family members often accompany patients, but should not be used as primary interpreters given the risk for biased interpretation.30 Educational sessions could provide an opportune setting for providers to learn how their patients’ cultural values may affect their beliefs about cancer and preferences regarding their treatment.30
Pamphlets
The use of informational pamphlets can also be an effective method of patient education for those undergoing RT. These can provide concise and detailed information about radiation treatment and side effects in a medium that can be distributed quickly and relatively inexpensively. Although certain patients may prefer printed materials, pamphlets can also be produced electronically and sent to patients via email or uploaded to their patient portal, allowing for decreased environmental impact, greater reach, and faster delivery compared with printed materials.31
A significant drawback of pamphlets is that they can be difficult for some patients to understand, particularly those with literacy limitations. Furthermore, pamphlets cannot offer the same level of personalization that an interactive discussion with a radiation oncologist, physicist, or therapist can provide. As a result, it can be difficult for patients to gain a full understanding of the risks and benefits of their treatment from pamphlets alone. Table 1 discusses advantages and disadvantages associated with each education modality discussed.
Clinical Application
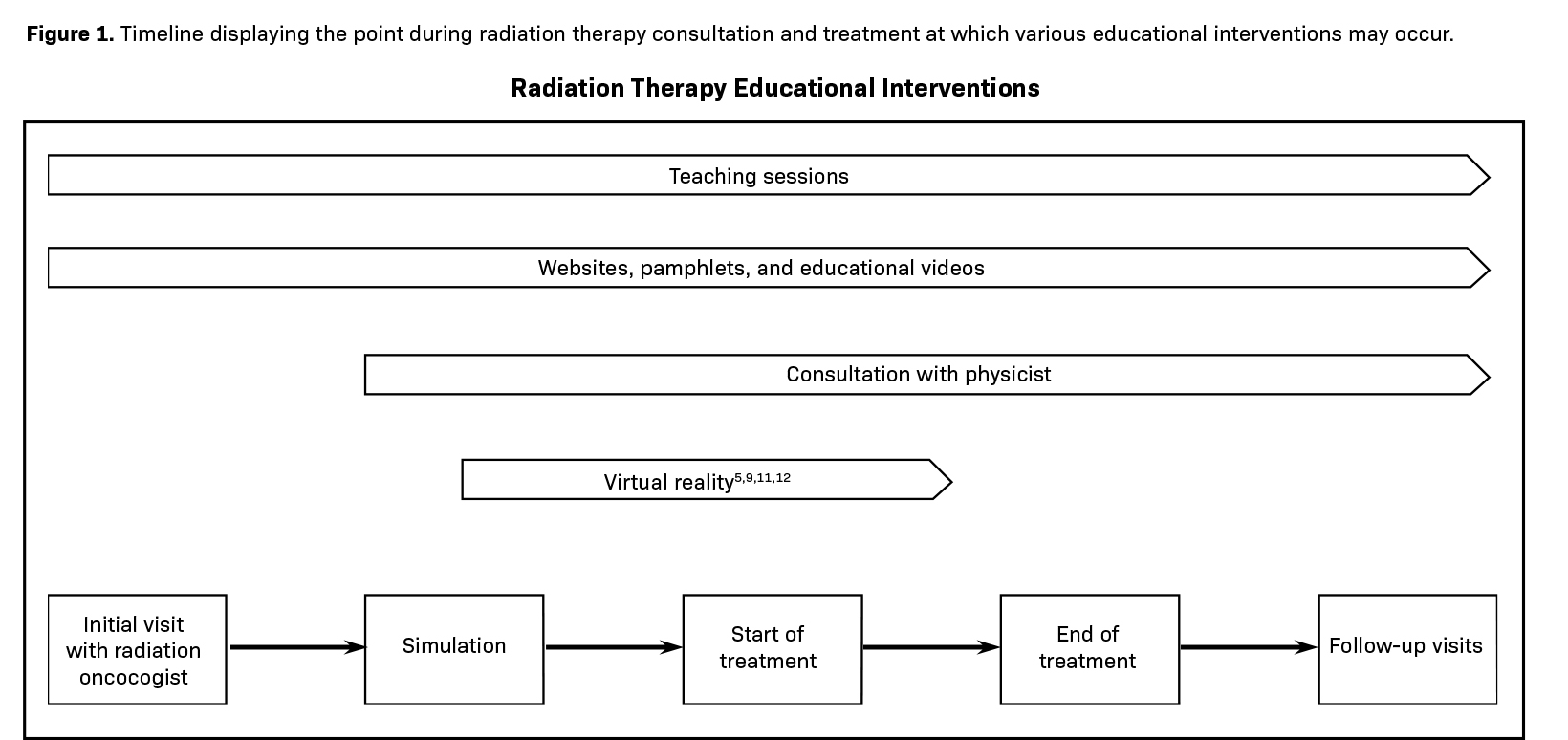
RT is a complex process that requires a multidisciplinary team for safe, effective execution. After the initial visit with a radiation oncologist, and once patients decide to pursue radiation treatment, they undergo simulation imaging with unique positioning considerations for optimal treatment. Planning may be modified and reassessed due to anatomic shifts. Once the planning and quality assurance process is complete, RT delivery begins.32 Patient education intervention has been implemented in many instances throughout the patient’s experience with the RT team. Physicist-patient consults, educational sessions with providers, and informational pamphlets have been provided directly before or after simulation sessions and before beginning treatment.22,28,29 Other educational modalities, such as videos, have been utilized prior to initial visits to establish a baseline understanding for patients.14
Conclusion
Patients receiving RT often experience emotional distress and anxiety.33 These emotions can be exacerbated by unfamiliarity and lack of understanding about RT. To address patient concerns and improve quality of care, a multimodal approach to education should be used throughout the RT workflow. The modalities should be directed toward patient-specific needs while considering demographics, health literacy, and baseline knowledge. A multidisciplinary approach may also be implemented with the radiation oncologists, physicists, and nurses at different time points in the treatment plan. Studies have suggested that effective teaching must occur early and throughout the course of radiation.29
Accessibility can be improved for many methods addressing RT patient education. Despite their ongoing efforts, education modalities often do not conform to the patient’s health literacy.34 Tools such as websites and pamphlets should be revised at a seventh-ninth grade reading level to be accessible and effective for the general population. Furthermore, patients who do not primarily speak English will also have additional language barriers when applying the multiple education modalities. To increase accessibility, future work should include creating opportunities for language translation, whether that be provided by the modality itself (eg, a website presented in multiple languages) or by an interpreter for tools such as educational sessions. Patient preferences and convenience should also be considered when incorporating increased technological modalities (eg, an elderly patient meeting for an education session in person instead of via videoconferencing). To improve and advance education sessions and medical physicist participation in consultations, direct patient care experience is also necessary for providers.35 Specific tracks or programming can be implemented in health care training programs to educate radiation oncology providers on various patient education modalities.
Ultimately, the goal of patient education technologies is to improve patient understanding of radiation treatment and reduce anxiety. As modalities improve and diversify, more patients will gain access to tools best suited for their unique preferences and physical needs.
References
- Jaffray DA, Gospodarowicz MK. Radiation therapy for cancer. In: Gelband H, Jha P, Sankaranarayanan R, Horton S, eds. Cancer: Disease Control Priorities, Third Edition (Volume 3). The International Bank for Reconstruction and Development / The World Bank; November 1, 2015.
- Matsuyama RK, Lyckholm LJ, Molisani A, Moghanaki D. The value of an educational video before consultation with a radiation oncologist. J Cancer Educ. 2013;28(2):306-313. doi:10.1007/s13187-013-0473-1
- Schnitzler L, Smith SK, Shepherd HL, et al. Communication during radiation therapy education sessions: the role of medical jargon and emotional support in clarifying patient confusion. Pat Educ Couns. 2017;100(1):112-120. doi:10.1016/j.pec.2016.08.006
- Arya R, Ichikawa T, Callender B, et al. Communicating the external beam radiation experience (CEBRE): perceived benefits of a graphic narrative patient education tool. Pract Radiat Oncol. 2020;10(4). doi:10.1016/j.prro.2019.09.001
- Jimenez YA, Cumming S, Wang W, Stuart K, Thwaites DI, Lewis SJ. Patient education using virtual reality increases knowledge and positive experience for breast cancer patients undergoing radiation therapy. Supp Care Cancer. 2018;26(8):2879-2888. doi:10.1007/s00520-018-4114-4
- Kumar KA, Balazy KE, Gutkin PM, et al. Association between patient education videos and knowledge of radiation treatment. Int J Radiat Oncol Biol Phys. 2021;109(5):1165-1175. doi:10.1016/j.ijrobp.2020.11.069
- Schuller BW, Burch C, Casterton T, Crowther C, Fowler J, Stenmark MH. Precision patient education using a “flipped classroom” approach. J Appl Clin Med Phys. 2022;23(5)e13601. doi:10.1002/acm2.13601
- Pembroke M, Bradley J, Mueller M, Mollica M, Nemeth LS. Feasibility of breast radiation therapy video education combined with standard radiation therapy education for patients with breast cancer. Oncol Nurs Forum. 2021;48(3):279-290. doi:10.1188/21.ONF.279-290
- Wang LJ, Casto B, Luh JY, Wang SJ. Virtual reality-based education for patients undergoing radiation therapy. J Cancer Educ. 2022;37(3):694-700. doi:10.1007/ s13187-020-01870-7
- Zeguers M, de Haes HCJM, Zandbelt LC, et al. The information needs of new radiotherapy patients: How to measure? Do they want to know everything? And if not, why? Int J Radiat Oncol Biol Phys. 2012;82(1):418-424. doi:10.1016/j.ijrobp.2010.09.032
- Sulé-Suso J, Finney S, Bisson J, et al. Pilot study on virtual imaging for patient information on radiotherapy planning and delivery. Radiography. 2015;21(3):273-277. doi:10.1016/j.radi.2015.02.002
- Galvez J, Eisenhower M, England W, et al. An interactive virtual reality tour for adolescents receiving proton radiation therapy: proof-of-concept study. JMIR Perioper Med. 2019;2(1):e11259. Published 2019 Mar 5. doi:10.2196/11259
- Flockton A. Men’s experience of virtual simulation to aid patient education for radiation treatment to the prostate. J Med Imag Radiat Sci. 2017;48(1). doi:10.1016/j.jmir.2017.02.021
- Brock TP, Smith SR. Using digital videos displayed on personal digital assistants (PDAs) to enhance patient education in clinical settings. Int J Med Inform. 2007;76(11-12):829-835. doi:10.1016/j.ijmedinf.2006.09.024
- Hahn CA, Fish LJ, Dunn RH, Halperin EC. Prospective trial of a video educational tool for radiation oncology patients. Am J Clin Oncol. 2005;28(6):609-612. doi:10.1097/01.coc.0000182417.94669.a0
- Rosenberg SA, Francis DM, Hullet CR, et al. Online patient information from radiation oncology departments is too complex for the general population. Pract Radiat Oncol. 2017;7(1):57-62. doi:10.1016/j.prro.2016.07.008
- Teplinsky E, Ponce SB, Drake EK, et al. Online medical misinformation in cancer: distinguishing fact from fiction. JCO Oncol Pract. 2022;18(8):584-589. doi:10.1200/op.21.00764
- Cutilli CC, Bennett IM. Understanding the health literacy of America. Orthop Nurs. 2009;28(1):27-32. doi:10.1097/01.nor.0000345852.22122.d6
- Garland ME, Lukac D, Contreras P. A brief report: comparative evaluation of online Spanish and English content on pancreatic cancer treatment. J Cancer Educ. 2022. doi:10.1007/s13187-022-02171-x
- Villa Camacho JC, Pena MA, Flores EJ, et al. Addressing linguistic barriers to care: evaluation of breast cancer online patient educational materials for Spanish-speaking patients. J Am Coll Radiol. 2021;18(7):919-926. doi:10.1016/j.jacr.2021.02.001
- Kutner M, Greenberg E, Baer J. A first look at the literacy of America’s adults in the 21st Century. Accessed February 12, 2023. https://nces.ed.gov/NAAL/ PDF/2006470.PDF
- Atwood TF, Brown DW, Murphy JD, et al. Examining the effect of direct patient care for medical physicists: a randomized prospective phase III trial. Int J Radiat Oncol Biol Phys. 2023;115(1):224-232. https://doi.org/10.1016/j.ijrobp.2022.05.014
- Atwood TF, Brown DW, Juang T, et al. A review of patient questions from physicist-patient consults. J App Clin Med Phys. 2020;21(8):305-308. https://doi. org/10.1002/acm2.12942
- Burmeister J, Dominello MM, Soulliere R, et al. A direct patient-provider relationship with the medical physicist reduces anxiety in patients receiving radiation therapy. Int J Radiat Oncol Biol Phys. 2023;115(1):233-243. https://www.sciencedirect.com/science/article/pii/S036030162203437X. doi:10.1016/j. ijrobp.2022.10.011
- Hyun M, Hyun A. Respecting patient autonomy in radiation oncology and beyond. In: Ethics and Error in Medicine. Routledge; 2019:103-117.
- Halkett G, O’Connor M, Jefford M, et al. RT prepare: a radiation therapist-delivered intervention reduces psychological distress in women with breast cancer referred for radiotherapy. Br J Cancer. 2018;118(12):1549-1558. doi:10.1038/s41416-018-0112-z
- Halkett GKB, O’Connor M, Aranda S, et al. Pilot randomised controlled trial of a radiation therapist-led educational intervention for breast cancer patients prior to commencing radiotherapy. Sup Care Cancer. 2013;21(6):1725-1733. doi:10.1007/s00520-013-1719-5
- Magliozzi M, Cashell A, Ishmail N, Hill C, Velec M. Virtual integration of patient education in radiotherapy (VIPER). Tech Innov Patient Support Radiat Oncol. 2022;23:47-57. doi:10.1016/j.tipsro.2022.08.008
- Zaheer S, Gul RB, Bhamani SS, Memon MA. The effect of individualized education with support on breast cancer patients’ anxiety and depression during radiation therapy: a pilot study. Eur J Oncol Nurs. 2020;48:101826. https://www.sciencedirect.com/science/article/pii/S146238892030106X. doi:10.1016/j. ejon.2020.101826
- Chou F-Y, Kuang LY, Lee J, Yoo GJ, Fung L-C. Challenges in cancer self-management of patients with limited English proficiency. Asia-Pacific J Oncol Nurs. 2016;3(3):259-265. doi:10.4103/2347-5625.189815
- Jewitt N, Hope AJ, Milne R, et al. Development and evaluation of patient education materials for elderly lung cancer patients. J Cancer Educ. 2016;31(1):70-74. doi:10.1007/s13187-014-0780-1
- Green OL, Henke LE, Hugo GD. Practical clinical workflows for online and offline adaptive radiation therapy. Semin Radiat Oncol. 2019;29(3):219-227. doi:10.1016/j.semradonc.2019.02.004
- Canil T, Cashell A, Papadakos J, Abdelmutti N, Friedman AJ. Evaluation of the effects of pre-treatment education on self-efficacy and anxiety in patients receiving radiation therapy: a pilot study. J Med Imag Radiat Sci. 2012;43(4):221-227. doi:10.1016/j.jmir.2012.05.002
- Giannopoulos E, McBain S, Giuliani M, et al. Health literacy and radiation therapy:a current state assessment of patient education materials. J Cancer Educ. 2022. doi:10.1007/s13187-022-02208-1
- Brown DW, Atwood TF, Moore KL, et al. A program to train medical physicists for direct patient care responsibilities. J Appl Clin Med Phys. 2018;19(6):332-335. doi:10.1002/acm2.12472.
Citation
Goldman J, Lin KK, Londoño V, Hoffe SE . Personalizing Approaches to Patient Education Throughout the Radiation Oncology Workflow. Appl Radiat Oncol. 2023;(1):14-19.
March 21, 2023
