Strip alopecia in high-dose VMAT-based stereotactic radiosurgery
Images




CASE SUMMARY
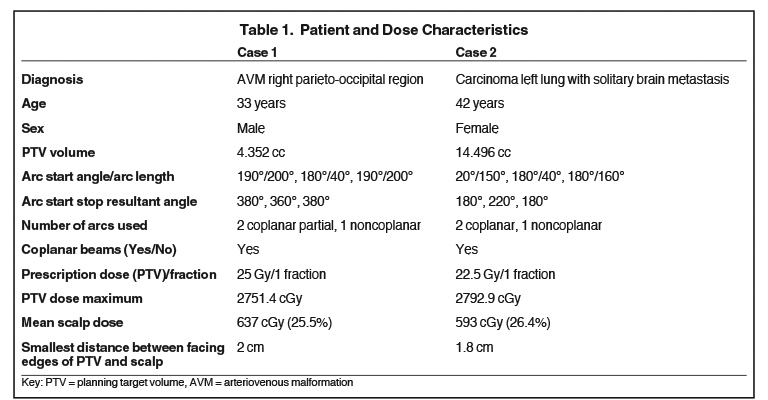
Between 2013 and 2019, 298 patients were treated with stereotactic radiation therapy (SRT) and radiosurgery (SRS) techniques in our center. The dose fractionation schedules ranged from 30 Gy in 5 fractions to 30 Gy in 1 fraction. A mixture of centrally and peripherally located lesions was seen among the treated patients. Of these patients, 2 reported alopecia over the beam locus. One patient had been treated for arteriovenous malformation (AVM) with a dose of 25 Gy, and the other had been treated for brain metastasis with a dose of 22.5 Gy, both with single-fraction treatments. All plans were meticulously evaluated before treatment delivery. For the first patient, at the time of treatment planning, the scalp was not contoured and the scalp dose was not optimized, whereas for the second patient, drawing of the scalp and its optimization were carried out. On retrospective analysis of the treatment plans, the scalp was contoured on the first patient and its mean dose was found to be 637 cGy (25.5%) of the prescription dose; for the second patient, this was 593 cGy (26.4%).
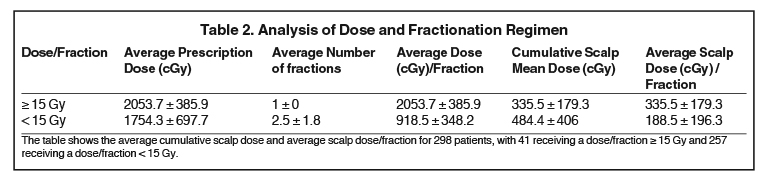
The manifestation of alopecia in a conventional 1.8 to 2 Gy per fraction treatment regimen is seen with a dose of at least 25 to 30 Gy.1,2 For single-fraction treatments, the typical dose is 5 to 8 Gy of biologically equivalent dose as per a conventional fractionation regimen.3-5 Analysis of all SRS/SRT patients in our center shows a mean scalp dose of 429.0 ± 344 cGy. In our patient subset, we did not come across any incidence of alopecia in patients who received < 15 Gy in a single fraction.
Our experience points to the in- creased risk of permanent or temporary alopecia in patients having peripherally located lesions when the delivered dose to the planning target volume (PTV) exceeds 20 Gy. We recommended delineation of the scalp and including it in dose opti mization.
METHOD
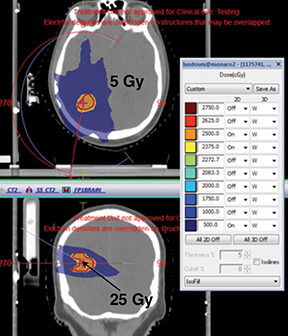
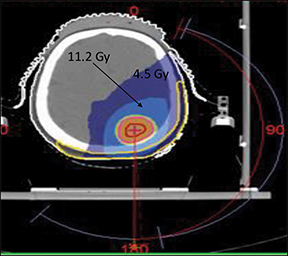
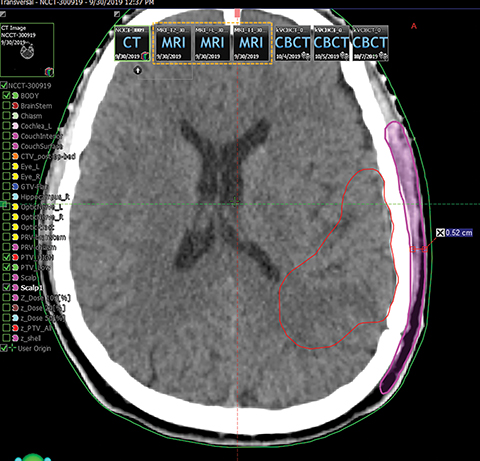
We started our stereotactic program in 2013 and have presented results in multiple forums.6-12 All patients were treated by a frameless stereotactic technique (SRS or SRT) using volumetric-modulated arc therapy (VMAT) on an Axesse (Elekta, Stockholm, Sweden) linear accelerator with a 4-mm multileaf collimator. Typically, SRS patients were treated by VMAT using 2 arcs (1 coplanar, 1 noncoplanar), and details of the planning strategy are presented in several studies.6-13 In this report, we present the finding of 2 unusual cases of strip alopecia for cranial stereotaxy as shown in Figures 1 and 2. Further, to evaluate the dose-effect relationship, a scalp organ at risk (OAR) was drawn. The scalp was drawn on the ipsilateral side in all the axial slices in which the lesion was visible. Furthermore, the scalp was extended manually 3 cm in anterior, posterior, cranial and caudal directions. (This was checked by placing a dummy lateral beam ipsilaterally and seeing the projection of the PTV and the scalp in a digitally reconstructed radiography [DRR] mode). We considered only the ipsilateral and partial scalp falling in the beam locus for optimization and dose evaluation.
Figure 3 presents the scalp as contoured in our clinic. No contouring guidelines are available for contouring the scalp. For the purpose of this study, the scalp was drawn as tissue between the outermost visible soft tissue (on the outside) and the bone/soft tissue interface on the inner side.
IMAGING FINDINGS
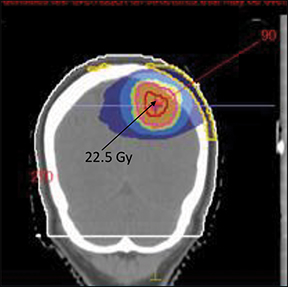
Figures 1 and 2 show an alopecia strip following SRS of the patients along with the dose-volume parameters of the radiation therapy plan. Both patients reported with strip alopecia after 2 months of their radiation therapy treatment. Two-year follow-up for case 1 revealed temporary alopecia with partial hair recovery. Initial evaluation of case 2 indicated permanent alopecia; follow-up data was not available as we lost contact with this patient.
Case 1 (Figure 1) was a 33-year-old man with AVM of the right parieto-occipital region. Digital-subtraction angiography showed a right 2.92 cm occipital nidus with extensive angiomatous changes. The patient received SRS treatment of 25 Gy in a single fraction.
Case 2 (Figure 2) was a 42-year-old woman with squamous cell carcinoma of the left lung. She received concurrent chemoradiation therapy followed by adjuvant chemotherapy. She developed solitary brain metastasis after a disease-free interval of 4 months, and treatment plans were made for a dose of 22.5 Gy in 1 fraction by SRS.
DIAGNOSIS
Case 1: AVM
Case 2: Brain metastasis
DISCUSSION
Over the years, SRS and SRT have become common practice in managing various benign and malignant brain conditions. The typical therapeutic doses are 12 to 30 Gy in 1 to 5 fractions. It is well-known that radiation therapy to the brain can lead to partial or total alopecia.3 Several investigators have tried to prevent this by various techniques, with mixed results.4,5
As with all patients, the treatment plans involved stringent physics quality assurance testing before treatment to ensure dose accuracy. Both patients had a single lesion located peripherally (close to the skull) and were treated with a single fraction (Table 1). In both cases, extensive alopecia was observed with complete loss of hair in the skull area corresponding to the paths of the treatment arcs. Our records of the 298 patients showed that alopecia was not observed in patients who had a centrally located lesion (eg, secretory pituitary adenoma cases treated with a single dose of 25 to 30 Gy). Similarly, when the prescription dose was < 15 Gy in a single fraction in both centrally and peripherally located lesions, the incidence of alopecia was not observed. The technique of determining a central vs peripheral tumor has been described in our early studies.6 The analysis of dose and fractionation regimen as a function of dose/fraction ≥ 15 Gy and dose/fraction < 15 Gy is presented in Table 2. The total number of patients was 298, with 41 patients receiving a dose/fraction ≥ 15 Gy and 257 receiving a dose/fraction < 15 Gy. The average cumulative scalp dose for ≥ 15 Gy/fraction and < 15 Gy/fraction regimens is 335.5 ± 179.3 cGy and 484.4 ± 406 cGy, respectively, whereas the average scalp dose (cGy)/fraction remains the same for the former group and reduces to 188.5 ± 196.3 cGy in the latter group. Drawing of the scalp and dose optimization were performed for 35 out of 41 patients in the dose/fraction ≥ 15 Gy group, and 200 out of 257 patients in the dose/ fraction < 15 Gy group. The scalp was not drawn if the patient was already bald. About half of the patients were from different countries and we lost follow-up with a few of them. Inland patients who received regular follow-up did not present with extensive strip alopecia other than these 2 cases.
After observing alopecia and its patterns, we contoured the partial scalp through which the beam entered with appropriate margins to determine whether any dose-effect relationship existed. The treatment planning data revealed that contoured strips of skull in the alopecia zone received a mean dose of 20 % of the prescription dose or less. The method section describes the technique of scalp drawing and its dose optimization. We drew a partial scalp since drawing a full scalp seems relatively infective in reducing dose to the relevant scalp area. The corresponding average absolute dose to the scalp was approximately 4 to 6 Gy for both patients. It is possible that actual surface doses were slightly different than doses estimated by the treatment planning system (TPS), but they are unlikely to be significantly higher. We did not perform in vivo dosimetry in our patients to confirm the TPS-estimated doses.
The phenomenon of alopecia observed in our cases is intriguing and surprising. VMAT arc-based treatment is an efficient technique of delivering treatment in a short span, causing the least patient discomfort. We used 2 noncoplanar arcs with large arc lengths, mainly aimed at increasing conformity and decreasing scalp dose. Despite these efforts, alopecia occurred. Our experience shows that one must be careful while treating peripherally located brain lesions with an SRS dose exceeding 20 Gy using a double-arc VMAT technique since there is an increased likelihood of hair loss even with the most meticulous planning and dose constraints to the scalp. The resultant alopecia is not patchy but continuous in nature and follows the VMAT arc pattern. A possible suggestion to avoid this strip alopecia is to use multiple smaller fields or to use a full arc (360 degrees) at the time of treatment planning. However, a standard solution for avoiding alopecia is not yet available.
CONCLUSION
We present two atypical cases of alopecia in patients treated with VMAT-based, single-fraction SRS for peripherally located tumors. All precautions should be taken to avoid alopecia for hypofractionated treatment—especially cranial stereotaxy—to avoid cosmetic disfigurement. Further study is required to establish the causal relationship between alopecia and dose/delivery technique.
REFERENCES
- Lawenda BD, Gagne HM, Gierga DP et al. Permanent alopecia after cranial irradiation: dose–response relationship. Int J Radiat Oncol Biol Phys. 2004;60(3):879-887.
- Shakespeare TP, Dwyer M, Mukherjee R, Yeghiaian-Alvandi R, Gebski V. Estimating risks of radiotherapy complications as part of informed consent: the high degree of variability between radiation oncologists may be related to experience. Int J Radiat Oncol Biol Phys. 2002;54(3):647-653.
- Severs GA, Griffin T, Werner-Wasik M. Cicatricial alopecia secondary to radiation therapy: case report and review of the literature. Cutis. 2008;81:147-153.
- De Puysseleyr, Van De Velde J, Speleers B, et al. Hair-sparing whole brain radiotherapy with volumetric arc therapy in patients treated for brain metastases: dosimetric and clinical results of a phase II trial. Radiat Oncol. 2014;9:170.
- Ting J, Thomas CR, McClure JA, Scarbrough TJ: “Alopecia-less” whole brain radiotherapy (WBRT) via IMRT: preliminary experience and outcomes. Int J Radiat Oncol Biol Phys. 2005;63:S263-S264.
- Sarkar B, Munshi A, Manikandan A, Anbazhagan S, Ganesh T, Mohanti BK. Standardization of volumetric modulated arc therapy based frameless stereotactic technique using a multidimensional ensemble aided knowledge-based planning. Med Phys. 2019;46(5):1953-1962.
- Munshi A, Sarkar B, Roy S, Ganesh T, Mohanti BK. Dose fall-off patterns with volumetric modulated arc therapy and three-dimensional conformal radiotherapy including the “organ at risk” effect. Experience of linear accelerator-based frameless radiosurgery from a single institution. Cancer/Radiothér. 2019;23(2):138-146.
- Sarkar B, Ray J, Ganesh T, et al. Methodology to reduce 6D patient positional shifts into a 3D linear shift and its verification in frameless stereotactic radiotherapy. Phys Med Biol. 2018;63(7):075004.
- Sarkar B, Pradhan A, Munshi A. Do technological advances in linear accelerators improve dosimetric outcomes in stereotaxy? A head-on comparison of seven linear accelerators using volumetric modulated arc therapy-based stereotactic planning. Indian J Can. 2016;53(1):166.
- Sarkar B, Pradhan A, Munshi A, Roy S, Ganesh T, Mohanti B. EP-1685: influence of flat, flattening filter free beam model and different MLCs on VMAT based SRS/SRT. Radiother Oncol. 2016;119:S787.
- Sarkar B, Ganesh T, Manikandan A, et al. Rotation corrected setup margin calculation for stereotactic body radiation therapy in dual imaging environment. Abstract #43679 presented at the American Association of Physicists in Medicine Annual Meeting & Exhibition; July 14-18, 2019; San Antonio, TX.
- Sarkar B, Munshi A, Krishnankutty S, Ganesh T, Kalyan MB. Positional errors in linear accelerator based frameless cranial stereotaxy: a note of caution. J BUON. 2017;22(6):1606.
- Sarkar B, Munshi A, Ganesh T, et al. Rotational positional error corrected intrafraction set‐up margins in stereotactic radiotherapy: a spatial assessment for coplanar and non-coplanar geometry. Med Phys. 2019; 46(11)4749-4754.
Citation
Munshi A, Sarkar B, Vaishya S, Bansal K, Rastogi K, Ganesh T, Mohanti BK. Strip alopecia in high-dose VMAT-based stereotactic radiosurgery. Appl Radiat Oncol. 2019;(4):45-48.
December 27, 2019
