Technology TrendsHead & Neck cancer
Technology Trends: Updates in IMRT, VMAT of the head and neck
Images
Head and neck cancers refer to a group of cancers of the oral cavity (mouth), nose, pharynx, larynx, lip or sinuses. While rare, accounting for 3% of all cancers in the United States or nearly 46,000 new cases each year,1 most head and neck cancers begin in the squamous cells that line mucosal surfaces in the mouth, nose and throat. 2 The 2 most important risk factors for these type cancers are tobacco use—including smokeless or chewing tobacco—and alcohol consumption. Infection by the human papillomavirus (HPV) is also believed to increase risk, specifically the HPV-16 genotype.1,2
Intensity-modulated radiation therapy (IMRT) is growing in use to treat cancer and tumors in more complicated areas of the body, such as the head and neck. It is well accepted and has been shown in the literature that a high-precision, more targeted delivery of external-beam radiation can improve treatment outcomes and tumor targeting, with less severe side effects.
When Daniel J. Haraf, MD, professor of Radiation and Cellular Oncology and Medical Director, Radiation Oncology, at The University of Chicago Medicine, began using IMRT in 1998-1999, no textbooks existed to guide him in planning. Today, he notes, manuals and reference guides from the American Society for Radiation Oncology (ASTRO) help radiation oncologists avoid critical structures and understand dose tolerances for organs and tissues.
“IMRT is a tool and a means to an end,” Dr. Haraf says. “The end [goal] is to get adequate radiation to where the cancer is lurking while limiting dose to normal structures. In a perfect world, we would only give radiation where it is needed and miss areas where it is not needed — it’s all about tradeoffs.”
Because of the many subtleties in developing an IMRT plan for head and neck cancer, it is important to know how the cancer is unique in each individual. IMRT, Dr. Haraf says, helps him do a better job of individualizing treatment. Individualized treatment plans also can benefit HPV-positive patients, who are at a higher risk for head and neck cancers, says Ping Xia, PhD, department head of medical physics at The Cleveland Clinic Foundation and an Applied Radiation Oncology advisory board member. Dr. Xia has been actively developing treatment planning techniques for head and neck cancer patients for over 15 years.
“HPV impacts the treatment because [these patients] are more sensitive to the radiation. We can de-intensify treatment for patients who are HPV positive, thus reducing treatment-related toxicity,” says Dr. Xia, noting that HPV-positive head and neck cancer patients tend to be younger and appear to have better outcomes.
An early adopter of IMRT and volumetric-modulated arc therapy (VMAT) for treating head and neck cancer, Dr. Xia serves as a physics co-primary investigator of NRG-HN002: A Randomized Phase II Trial for Patients with p16 Positive, Non-Smoking Associated, Locoregionally Advanced Oropharyngeal Cancer, NCT02254278. This trial is investigating a de-intensified treatment regimen for patients with HPV-positive oropharyngeal cancer.3
Reducing side effects is an important benefit of IMRT compared to conventional radiotherapy. A pivotal study conducted by researchers at the Royal Marsden Hospital and the Institute of Cancer Research in London, and published in the February 2011 issue of Lancet Oncology, was one of the first studies to compare IMRT to conventional radiotherapy.1 The goal of the prospective, randomized study was to determine whether IMRT could spare salivary glands and reduce xerostomia, also known as dry mouth from reduced or absent saliva flow. The authors reported a “significant reduction of radiation-induced xerostomia” in patients treated with IMRT compared to those who received conventional radiotherapy. The IMRT treatments were designed to spare the parotid gland—the major salivary gland. The authors also reported improved salivary flow and better quality of life in patients who received IMRT.4
Difficulty swallowing is another potential side effect, notes Dr. Xia. Today, radiation oncologists and medical physicists aim to protect the larynx and other structures that affect swallowing during IMRT treatments. “Our knowledge is progressing. When we first started IMRT in 1997, we focused mostly on a few critical structures—the brain stem or spinal cord and parotid glands,” she says. “In our current IMRT planning, the number of organs or structures we spare in our planning is 30, and this includes the larynx and oral cavity. Before, the patient had to live with these side effects; now we try to treat their disease and also improve their quality of life.”
In addition to reducing toxicity to healthy organs and tissues, IMRT can improve survival rates. A 2014 study published in Cancer analyzed the Surveillance, Epidemiology, and End Results (SEER)-Medicare database to determine cause-specific survival (CSS) for head and neck patients treated with IMRT compared to non-IMRT treatment delivery methods. The goal was to determine whether the widely accepted, yet more expensive, IMRT benefitted patients or exposed them to more risk regarding outcomes.
A total of 3,172 patients were identified with a median follow-up of 40 months. In the analysis, the authors reported that patients treated with IMRT had a statistically significant improvement in CSS (38.9%) compared to non-IMRT treated patients (18.9%). Even when accounting for variables such as account diagnosis, marriage, rural vs. urban setting, income and other factors, patients treated with IMRT still had a CSS benefit.5 As a result of the analysis, the authors suggest that IMRT may improve patient outcomes in those with head and neck cancers. (See Figure 1 for an example of IMRT results in this patient population.)
Recently, a small sample-size study examined brain-sparing methods for IMRT in 10 patients with head and neck cancer. Both a hippocampus-sparing plan and a brain/hippocampus-sparing plan were generated, and dose volume histograms (DVHs) and dose difference maps were compared. In 8 of 10 cases in both types of treatment plans, the authors detected significant reductions in hippocampal doses relative to conventional plans. They suggest that IMRT has a high probability of reducing neurocognitive function decline in head and neck cancer patients, and that results could be translated into a future clinical trial.6
Dr. Haraf has become a widely recognized leader in combining IMRT with chemotherapy for treating head and neck cancers. Efforts to decrease toxicity to critical organs, and thereby lower side effects of radiation treatment, are increasingly important. Combining chemotherapy with IMRT is an important step in this direction, he says.
Historically, head and neck cancers had a survival rate of 30% to 40%. With concomitant chemotherapy and radiation therapy, survival rates have increased to > 50 %, he says. In fact, Dr. Haraf is optimistic that about 70% of current head and neck cancer cases could be cured using radiation therapy and chemotherapy. IMRT has helped increase survival by better targeting cancer while limiting toxicity.
At the 2015 American Society of Clinical Oncology (ASCO) Meeting held May 29 to June 2 in Chicago, Dr. Haraf was co-author of a poster on a study that examined whether radiation therapy volumes could be reduced in patients who responded to induction chemotherapy.7 The study examined the use of response-adapted volume de-escalation (RAVD) to guide a reduction in radiation therapy for chemotherapy responders, and found that outcomes were not compromised, and long-term toxicity could potentially improve.7
While IMRT has been shown in the literature to improve survival and quality of life while reducing side effects, Dr. Xia uses VMAT in the majority of head and neck cancer patients. She finds that VMAT provides more freedom in the beam angle and offers more variables in the treatment-planning process to better avoid critical structures while delivering more targeted, higher doses to the tumor site.
“VMAT is really an advanced form of IMRT and, clinically, the quality of the plan is better than a conventional step-and-shoot IMRT,” Dr. Xia says. “Most important is the gain in delivery time. I remember in 1997 we had a 30 minute on-beam time. Now with VMAT, it is 5 minutes.”
In addition to the higher efficiency and added patient convenience of the VMAT treatment plans, Dr. Xia and her team at The Cleveland Clinic Foundation also perform more daily image-guided radiotherapy using a cone-beam CT equipped on the linear accelerator.
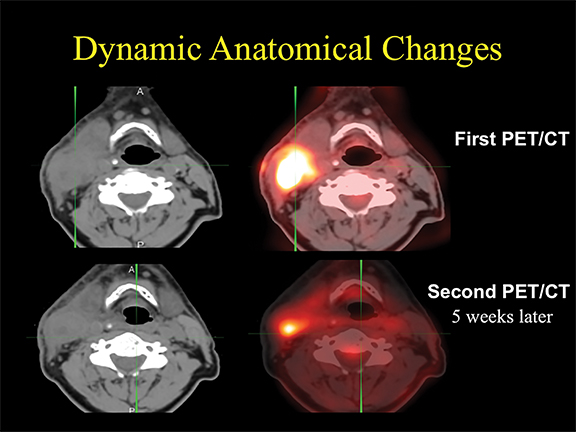
“Two things happen to head and neck patients during treatment: With chemotherapy, they tend to lose weight. Also, the tumor responds to treatment and shrinks during radiation therapy,” she explains. For most patients who receive radiotherapy, only one plan is designed for the entire treatment course. Yet, performing adaptive radiotherapy on all patients would require extensive resources—and the benefits are not yet clinically evident. Through research, Dr. Xia hopes to identify patients who would benefit the most from this advanced treatment.
References
- American Cancer Society. Cancer Facts & Figures 2015. http://www.cancer.org/research/cancerfactsstatistics/cancerfactsfigures2015/. Accessed May 7, 2015.
- National Cancer Institute. http://www.cancer.gov/cancertopics/types/head-and-neck/head-neck-fact-sheet. Accessed May 7, 2015.
- NRG-HN002: A Randomized Phase II Trial for Patients with p16 Positive, Non-Smoking Associated, Locoregionally Advanced Oropharyngeal Cancer, NCT002254278. https://www.nrgoncology.org/Clinical-Trials/NRG-HN002 Accessed May 7, 2015.
- Nutting CM, Morden JP, Harrington, KJ, et al. Parotid-sparing intensity modulated versus conventional radiotherapy in head and neck cancer (PARSPORT): a phase 3 multicentre randomised controlled trial. Lancet Oncol. 2011;12:127-136.
- Beadle BM, Kai-Ping L, Elting LS, et al. Improved survival using intensity-modulated radiation therapy in head and neck cancers. Cancer. 2014; 120:702-710.
- Dunlop A, Welsh L, McQuaid D, et al. Brain-sparing methods for IMRT of head and neck cancer. PLOS One. March 17, 2015.
- Villaflor VM, Cohen EEW, Melotek JM, et al. Response-adapted volume de-escalation (RAVD) of radiotherapy (RT) using induction chemotherapy (IC) in locally advanced head and neck squamous cell cancer (LA-HNSCC). J Clin Oncol. 2015;33(suppl; abstr 6050).
