AI Predicts Breast Cancer Risk Better Than Standard Clinical Risk Model
 Artificial intelligence (AI) algorithms outperformed the standard clinical risk model for predicting the five-year risk for breast cancer using thousands of mammograms in a large study published in Radiology.
Artificial intelligence (AI) algorithms outperformed the standard clinical risk model for predicting the five-year risk for breast cancer using thousands of mammograms in a large study published in Radiology.
A woman's risk of breast cancer is typically calculated using clinical models such as the Breast Cancer Surveillance Consortium (BCSC) risk model, which uses self-reported and other information on the patient—including age, family history of the disease, whether she has given birth, and whether she has dense breasts—to calculate a risk score.
"Clinical risk models depend on gathering information from different sources, which isn't always
available or collected," said lead researcher Vignesh A. Arasu, M.D., Ph.D., a research scientist and practicing radiologist at Kaiser Permanente Northern California. "Recent advances in AI deep learning provide us with the ability to extract hundreds to thousands of additional mammographic features."
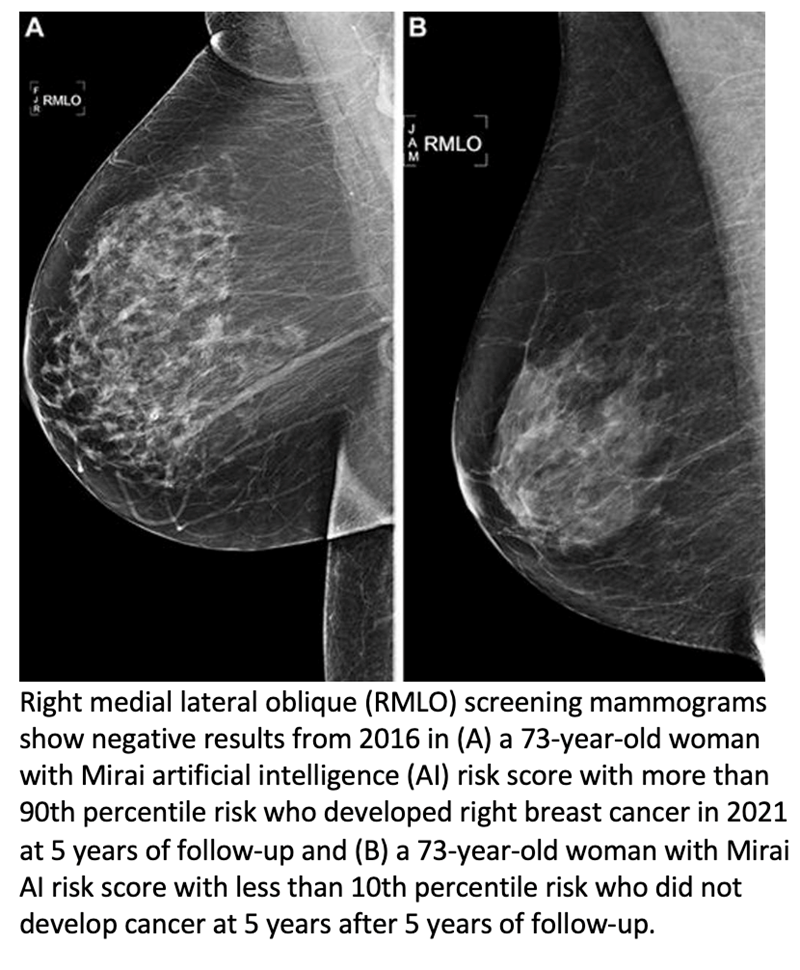
In the retrospective study, Dr Arasu used data associated with negative (showing no visible evidence of cancer) screening 2D mammograms performed at Kaiser Permanente Northern California in 2016. Of the 324,009 women screened in 2016 who met eligibility criteria, a random sub-cohort of 13,628 women was selected for analysis. Additionally, all 4,584 patients from the eligibility pool who were diagnosed with cancer within five years of the original 2016 mammogram were also studied. All the women were followed until 2021.
"We selected from the entire year of screening mammograms performed in 2016, so our study population is representative of communities in Northern California," Dr Arasu said.
The researchers divided the five-year study period into three time periods: interval cancer risk, or incident cancers diagnosed between 0 and 1 years; future cancer risk, or incident cancers diagnosed from between one and five years; and all cancer risk, or incident cancers diagnosed between 0 and 5 years.
Using the 2016 screening mammograms, risk scores for breast cancer over the five-year period were generated by five AI algorithms, including two academic algorithms used by researchers and three commercially available algorithms. The risk scores were then compared to each other and to the BCSC clinical risk score.
"All five AI algorithms performed better than the BCSC risk model for predicting breast cancer risk at 0 to 5 years," Dr Arasu said. "This strong predictive performance over the five-year period suggests AI is identifying both missed cancers and breast tissue features that help predict future cancer development. Something in mammograms allows us to track breast cancer risk. This is the 'black box' of AI."
Some of the AI algorithms excelled at predicting patients at high risk of interval cancer, which is often aggressive and may require a second reading of mammograms, supplementary screening or short-interval follow-up imaging. When evaluating women with the highest 10% risk as an example, AI predicted up to 28% of cancers compared to 21%predicted by BCSC.
Even AI algorithms trained for short time horizons (as low as 3 months) were able to predict the future risk of cancer up to five years when no cancer was clinically detected by screening mammography. When used in combination, the AI and BCSC risk models further improved cancer prediction.
"We're looking for an accurate, efficient and scalable means of understanding a women's breast cancer risk," Dr Arasu said. "Mammography-based AI risk models provide practical advantages over traditional clinical risk models because they use a single data source: the mammogram itself."
Dr Arasu said some institutions are already using AI to help radiologists detect cancer on mammograms. A person's future risk score, which takes seconds for AI to generate, could be integrated into the radiology report shared with the patient and their physician.
"AI for cancer risk prediction offers us the opportunity to individualize every woman's care, which isn't systematically available," he said. "It's a tool that could help us provide personalized, precision medicine on a national level."