IBA, KUMC to Collaborate on FLASH Research
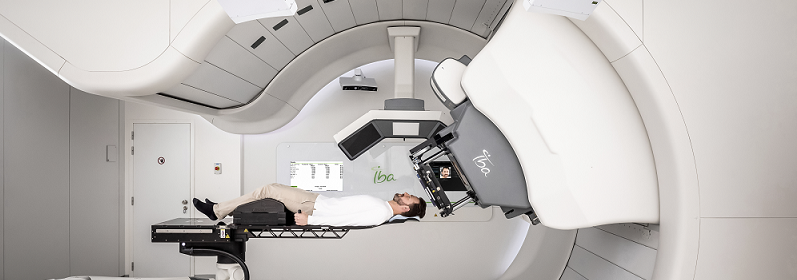 IBA announced a research collaboration agreement with the University of Kansas Medical Center (KUMC) to advance preclinical research into the use of ConformalFLASH technology using an IBA ProteusONE machine. The preclinical evaluation will be focused on skin and muscular normal tissue sparing after proton FLASH irradiation.
IBA announced a research collaboration agreement with the University of Kansas Medical Center (KUMC) to advance preclinical research into the use of ConformalFLASH technology using an IBA ProteusONE machine. The preclinical evaluation will be focused on skin and muscular normal tissue sparing after proton FLASH irradiation.
The two organizations published a joint abstract, “Experimental demonstration of 360nA FLASH proton beam current via synchrocyclotron using IBA ProteusONE,” during the Proton Therapy Co-Operative Group (PTCOG) Congress 2023, which took place in Madrid, Spain, in June. The collaboration announced today will facilitate a deepening of the research partnership between IBA and KUMC, as they look to develop ConformalFLASH in a clinical ProteusONE treatment room.
Olivier Legrain, Chief Executive Officer of IBA, commented, “We are excited to partner with the University of Kansas Medical Center, comprising some of the brightest minds in the field of radiation oncology who have consistently pushed the boundaries of what is possible. This collaboration brings together a synergy of expertise and a shared passion for exploring the potential of FLASH radiotherapy and its translation to the clinic. We are eager to continue pushing the boundaries of knowledge on FLASH and sharing this expertise with our large community of IBA centers.”
Ronald Chen, MD, Chair of the Department of Radiation Oncology at The University of Kansas Medical Center, added, “As an NCI-designated comprehensive cancer center, The University of Kansas Cancer Center at KUMC is committed to being a leader in cancer-related research. FLASH therapy has the potential to transform cancer care. Our team of physician scientists, physicists and radiobiologists is excited to collaborate with IBA to lead preclinical and clinical research in this area, so FLASH can be a clinical reality to help cancer patients in the not-so-distant future.”
ConformalFLASH is a ultra-high dose rate proton delivery using the Bragg peak, combining the biological tissue-sparing effects of FLASH with the physics properties of the proton Bragg peak. This technology distinguishes itself from electron FLASH machines, that are currently limited to deliver FLASH dose rates to superficial tumors, and protons transmission FLASH delivery, which has reduced conformality and higher integral doses compared to
ConformalFLASH.
FLASH irradiation has the potential to dramatically change the landscape of radiotherapy and patient cancer care by enhancing the therapeutic window with less toxicity and possibility to escalate the dose with shorter treatment. FLASH, defined as radiation delivery at ultra-high dose rates (40-60Gy/s), has been shown in preclinical research to spare normal tissue toxicity while maintaining an equivalent anti-tumor efficacy.
