MRI-guided SBRT Reduces Genitourinary Toxicity in Men Treated for Prostate Cancer
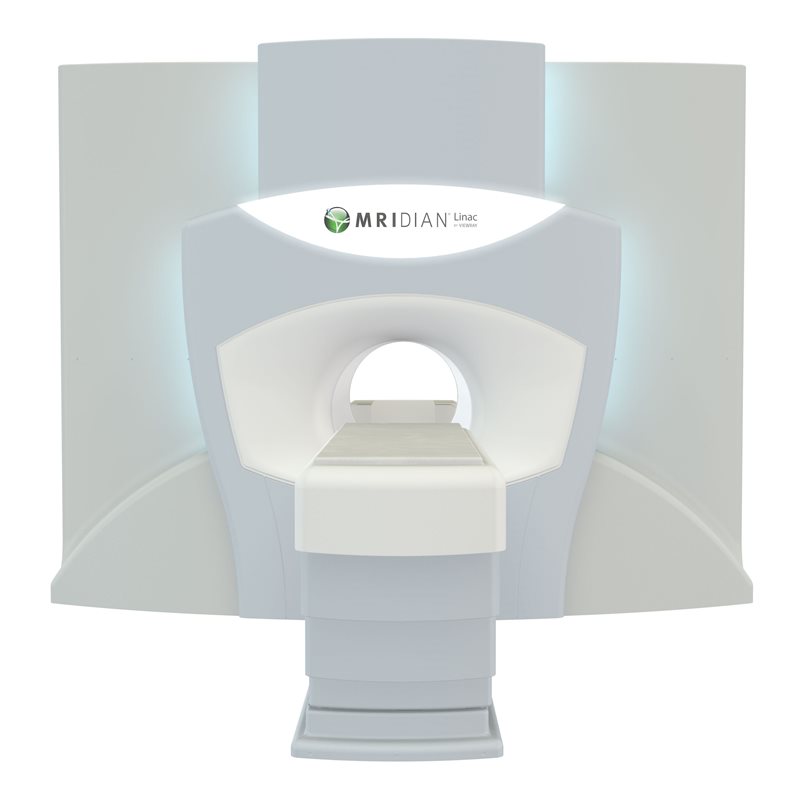 Interim data being presented at the 2022 American Society of Clinical Oncology (ASCO) Genitourinary (GU) Cancers Symposium indicates that MRI-guided SBRT is superior to CT-guided SBRT in reducing toxicities and side effects of treating prostate cancer. The single center, Phase III randomized MIRAGE trial, led by UCLA, compared MRIdian MRI-guided vs. CT-guided SBRT for localized prostate cancer. Interim analysis of the primary endpoint signaled the superiority of MRIdian MRI-guided SBRT with a significant reduction in acute grade ≥2 GU toxicity in men receiving MRI-guided SBRT over those receiving CT-guided SBRT.
Interim data being presented at the 2022 American Society of Clinical Oncology (ASCO) Genitourinary (GU) Cancers Symposium indicates that MRI-guided SBRT is superior to CT-guided SBRT in reducing toxicities and side effects of treating prostate cancer. The single center, Phase III randomized MIRAGE trial, led by UCLA, compared MRIdian MRI-guided vs. CT-guided SBRT for localized prostate cancer. Interim analysis of the primary endpoint signaled the superiority of MRIdian MRI-guided SBRT with a significant reduction in acute grade ≥2 GU toxicity in men receiving MRI-guided SBRT over those receiving CT-guided SBRT.
The poster, titled "Magnetic resonance imaging-guided versus computed tomography-guided stereotactic body radiotherapy for prostate cancer (MIRAGE): Interim analysis of a phase III ran-domized trial" and authored by Amar Kishan, MD, Associate Professor and Chief of the Genitourinary Oncology Service at UCLA, will be showcased on Thursday, February 17 from 11:30 AM PT to 1:00 PM PT as part of the Prostate Cancer poster session. Following the poster session, Dr. Kishan (@AmarUKishan) will host a LIVE Twitter Q&A to answer questions about the interim findings. Those interested can join the conversation and post their questions using #MIRAGEQ&A.
The interim analysis of data from 100 patients eligible for evaluation (51 in the CT group and 49 in the MRI group) showed a statistically significant reduction in acute grade ≥2 GU toxicity in men receiving MRI-guided SBRT (47.1% in the CT group vs. 22.4% in the MRI group) and a significant reduction in acute grade ≥2 gastrointestinal (GI) toxicity in men receiving MRI-guided SBRT (13.7% in the CT group vs. 0% in the MRI group). Acute grade ≥2 GU toxicity can include adverse events range from frequent, urgent, or painful urination to pelvis pain, bladder spasms, or blood in the urine. Acute grade ≥2 GI toxicity can include adverse events ranging from diarrhea, discharge, or rectal/abdominal pain to abdominal distention or obstruction.
Patient-reported outcomes were measured using the International Prostate Symptom Score (I-PSS) and Expanded Prostate cancer Index Composite (EPIC-26). Patient reported urinary and bowel function metrics were better preserved at the 1-month time point with MRI-guidance, though this difference dissipates at the 3-month time point, potentially due to management of side effects.
"Beyond a reduction in the standardized metric of physician-scored toxicity, we also saw differences in one-month patient-reported urinary and bowel function metrics favoring the MRI-guidance arm. These data are highly indicative of less radiation dose being delivered to sensitive structures, such as the bladder, urethra, and rectum, with MRI-guidance," said Dr. Kishan. "Potential explanations for the magnitude of these results can be attributed to the real-time tissue tracking of actual anatomy and automatic gating of beam delivery, which thereby allows for tighter contours and treatment of smaller volumes. The high dose regions are significantly smaller for patients receiving MRI-guided SBRT."
Given the large primary endpoint signal seen, the study protocol was amended to reduce the projected sample size from 300 to 154, requiring half the number of patients while still maintaining 89% power to demonstrate superiority. Accrual of the MIRAGE trial (NCT04384770) was completed as of October 2021 and a final analysis for the primary endpoint is anticipated in early 2022.
"While the final results are still being analyzed, it is evident from our interim analysis that the benefit provided by MRI-guidance over CT-guidance for the delivery of SBRT for localized prostate cancer is projected to be large enough that we were able to cut the projected size of our trial in half. In fact, by the time this interim analysis was done, we had already enrolled enough patients to close the trial successfully," said Dr. Kishan. "In anticipation of the highly positive result implied by this interim analysis, we have now shifted to routinely offering MRI-guided SBRT at UCLA."