Novel CAR-T Therapy and Shorter Targeted Therapy Durations Show Promise for Leukemia Patients
 Researchers from The University of Texas MD Anderson Cancer Center presented positive clinical results from two studies at the 2024 American Society of Clinical Oncology (ASCO) Annual Meeting. The findings highlight strong remission and response rates and offer insights into improving treatment options for relapsed or refractory B-cell acute lymphoblastic leukemia (B-ALL) and acute myeloid leukemia (AML) in older or chemotherapy-ineligible patients.
Researchers from The University of Texas MD Anderson Cancer Center presented positive clinical results from two studies at the 2024 American Society of Clinical Oncology (ASCO) Annual Meeting. The findings highlight strong remission and response rates and offer insights into improving treatment options for relapsed or refractory B-cell acute lymphoblastic leukemia (B-ALL) and acute myeloid leukemia (AML) in older or chemotherapy-ineligible patients.
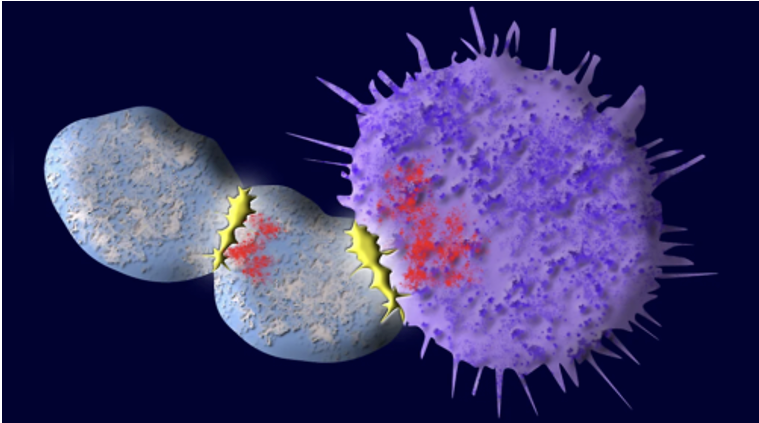
In one study presented, the novel anti-CD19 autologous chimeric antigen receptor (CAR) T cell therapy obecabtagene autoleucel (obe-cel) achieved durable remissions in 40% of patients with relapsed or refractory B-ALL without a subsequent stem cell transplant (SCT), according to results from the Phase Ib/II FELIX clinical trial presented today by Elias Jabbour, MD, professor of Leukemia.
At a median follow-up of 21.5 months, these patients were in ongoing remission without SCT or other therapies. The 12-month event-free survival (EFS) and overall survival (OS) rates were 49.5% and 61%, respectively.
Eighteen percent of patients, all with no measurable residual disease, went on to receive a SCT after obe-cel infusion. Of these patients, 55% had persistent CAR T cells present prior to transplant. The median time to SCT was 101 days after treatment.
The median EFS and 12-month EFS rate were identical between those who did and did not receive a SCT, and similar findings were observed when researchers assessed for OS. These results suggest that SCTs did not offer additional value for these patients and that obe-cel could be considered as a standalone treatment, Jabbour explained.
“We observed that persistence of CAR T cells and B-cell aplasia both were associated with improved event-free survival in patients treated with obe-cel,” Jabbour said. “These outcomes demonstrate a potential of a long-term plateau in the survival curve, which supports this therapy being considered as a standard-of-care for adults with relapsed or refractory B-ALL who currently have limited treatment options.” B-cell aplasia occurs when anti-CD19 CAR T cells kill CD19-expressing B-lymphocytes causing a patient to have an extremely low B-cell count.
The open-label, multi-center, single-arm trial treated 127 adult patients with relapsed or refractory B-ALL with obe-cel. Trial participants had lymphodepletion, an important step that kills existing T-cells to create a blank slate for CAR T cell therapy, followed by obe-cel infusion in split doses on days one and 10. Side effects were consistent with previous studies, and no new adverse effects were identified.
In the other study presented, shorter durations of venetoclax was found to yield similar response rates in AML. When combined with azacitidine, a 7-day course of venetoclax demonstrated similar remission rates and was more tolerable compared to the standard 28-day course for older or chemotherapy-ineligible patients with newly diagnosed AML. Results from the retrospective multi-center analysis were presented today by Alexandre Bazinet, MD, assistant professor of Leukemia.
Both groups had a composite complete remission rate of 72%, and the median OS for the shorter duration cohort was 11.2 months compared with 10.1 months for the longer duration cohort. Interestingly, OS with standard dosing was longer in patients without high-risk mutations, suggesting these patients have a more “sensitive” leukemia that responds well to more venetoclax exposure. Additionally, the 8-week mortality rate was significantly higher in the 28-day treatment group compared to the 7-day group at 16% vs 6%, respectively.
“Our findings suggest shorter courses of venetoclax for the treatment of AML may help reduce side effects and improve patients’ tolerability of treatment without compromising response rates,” Bazinet said. “Older patients tend to experience more side effects and often have additional medical issues which increases the risk of serious complications. It’s important to identify treatment options that can produce similar rates of remission and survival for these patients.”
In a retrospective analysis, researchers compared data from 82 patients treated with the shorter 7-day venetoclax course to that of 166 patients treated with the current recommended 28-day course. Responses were slower with the 7-day course compared to the standard course, often requiring more than one cycle to achieve the first response. However, most patients eventually responded with added cycles, resulting in an equal composite complete remission rate between the cohorts.
Researchers observed a significantly lower need for platelet transfusions and lower early mortality in patients receiving the 7-day course, suggesting the shorter course was more tolerable.
The study supports use of shorter courses of venetoclax in triplet regimens such as those being developed by MD Anderson researchers to treat older or chemotherapy-ineligible patients.