Prostate Cancer Patients Experience Fewer Side Effects With Image-Guided Adaptive Radiotherapy
 A technique known as magnetic resonance–guided daily adaptive stereotactic body radiotherapy (MRg-A-SBRT) can significantly enhance the safety of radiation therapy for patients with prostate cancer. By utilizing imaging technology as a guide, this approach enables clinicians to precisely target radiation beams at the prostate while minimizing exposure to nearby tissues in the bladder, urethra, and rectum. These findings emerged from a comprehensive analysis of all published clinical trials of MRg-A-SBRT, published in the journal Cancer.
A technique known as magnetic resonance–guided daily adaptive stereotactic body radiotherapy (MRg-A-SBRT) can significantly enhance the safety of radiation therapy for patients with prostate cancer. By utilizing imaging technology as a guide, this approach enables clinicians to precisely target radiation beams at the prostate while minimizing exposure to nearby tissues in the bladder, urethra, and rectum. These findings emerged from a comprehensive analysis of all published clinical trials of MRg-A-SBRT, published in the journal Cancer.
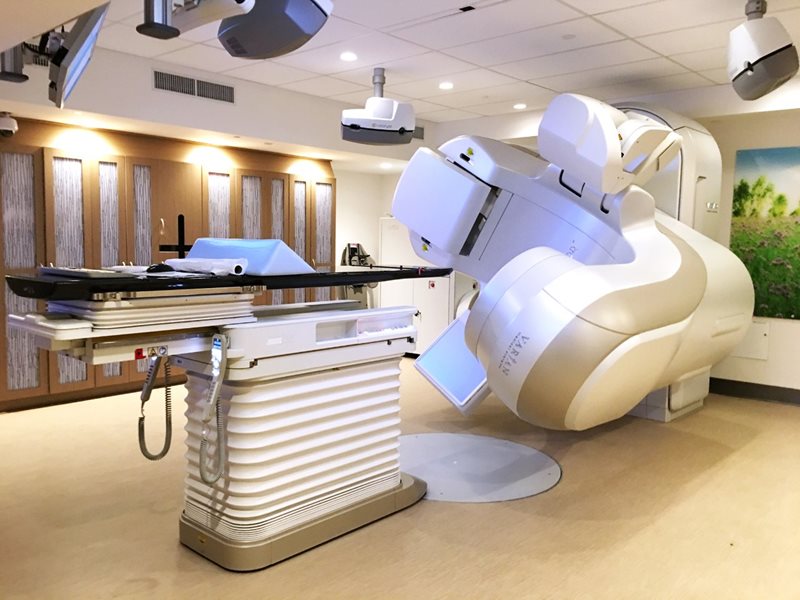
MRg-A-SBRT provides high-resolution images that allow for daily adjustments to a patient's radiation plan, accommodating any anatomical changes and facilitating real-time monitoring of the prostate's position during radiation treatment. This ensures that the radiation is accurately directed at the prostate, increasing treatment efficacy.
While MRg-A-SBRT is gaining popularity and has been tested in multiple clinical trials, it remains uncertain whether the technique, due to its additional time and resource requirements compared to standard procedures, yields discernible differences in clinical outcomes and side effects when compared to other radiation delivery methods. Further research is needed to comprehensively assess the impact of this advanced technique on patient outcomes and overall treatment efficacy.
Jonathan E. Leeman, MD, along with his colleagues from the Dana-Farber Cancer Institute and Brigham and Women's Hospital, conducted a thorough investigation into the effectiveness of MRg-A-SBRT for prostate cancer treatment. To accomplish this, they conducted a comprehensive search of medical literature for prospective studies that had tested MRg-A-SBRT. Combining data from 29 clinical trials involving a total of 2,547 patients, they compared the side effects of MRg-A-SBRT with a more conventional treatment method that utilized computed tomography guidance but did not involve daily adjustments as in MRg-A-SBRT.
The results of their analysis revealed that MRg-A-SBRT led to significantly fewer urinary and bowel side effects in the short term following radiation treatment. Specifically, there was a remarkable 44% reduction in urinary side effects and an impressive 60% reduction in bowel side effects.
Dr. Leeman stated that this study is the first of its kind to directly compare the benefits of MR-guided adaptive prostate radiation with a more standard and conventional form of radiation. The findings strongly support the use of MRg-A-SBRT as an effective treatment option for managing prostate cancer.
An accompanying editorial discusses the analysis’ findings, weighs the potential benefits and shortcomings of adopting this treatment strategy for patients, and questions the value of broad adoption.