Volume Doubling Times in Part-Solid Lung Adenocarcinomas Have Greater Prognostic Importance
 In resected lung adenocarcinomas manifesting as part-solid lesions, volume doubling times (VDTs) less than 200 days was the only VDT metric significantly associated with both recurrence-free survival (RFS) and overall survival (OS), according to research published in the American Journal of Roentgenology (AJR).
In resected lung adenocarcinomas manifesting as part-solid lesions, volume doubling times (VDTs) less than 200 days was the only VDT metric significantly associated with both recurrence-free survival (RFS) and overall survival (OS), according to research published in the American Journal of Roentgenology (AJR).
“Assessment of the growth rates of part-solid lesions should focus on these lesions’ solid components, aligning with the recognized greater biologic aggressiveness of such components,” wrote corresponding author Sang Min Lee, MD, from the Research Institute of Radiology at South Korea’s University of Ulsan College of Medicine in Seoul.
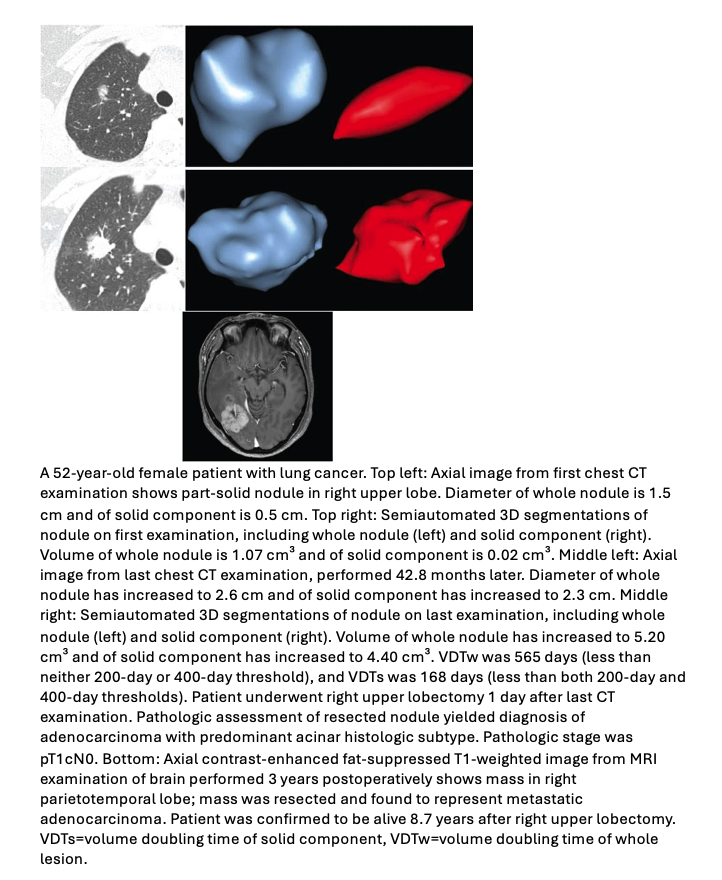
Lee et al.’s AJR manuscript studied 122 patients (mean age, 64; 53 men, 69 women) with resected lung adenocarcinoma manifesting as a part-solid lesion who underwent at least two preoperative chest CT examinations showing either solid-component growth or at least 2 years of stability. Semiautomated software was used to perform 3D segmentations of whole lesions and their solid components—to derive corresponding whole-lesion and solid-component volumes. These volumes were used to compute for each patient VDT for the whole lesion (VDTw) and the lesion’s solid component (VDTs). For 81 patients in whom the lesion’s ground-glass component increased, VDT of the ground-glass component (VDTgg) was calculated, subtracting the solid-component volume from whole-lesion volume to derive the ground-glass component volume. The prognostic utility of VDTw, VDTs, and VDTgg (each as continuous variables and as binary variables at 200-day and 400-day cutoffs) for RFS and OS were evaluated using Cox proportional hazard models, adjusting for age, sex, and clinical variables associated with lung cancer survival.
Ultimately, in these lung adenocarcinomas displaying as part-solid lesions, a VDT of the solid component fewer than 200 days was the only VDT evaluated metric on preoperative chest CT examinations to show significant independent associations with RFS (HR=3.68; 95% CI, 1.57–8.62; p=.003) and OS (HR=3.27; 95% CI, 1.01–10.52; p=.047) alike.