Intrarterial Radionuclide Therapy Effective and Safe for Advanced Meningioma Patients
 Radionuclide therapy delivered directly to an artery is feasible and safe for patients with advanced meningioma, according to new research published in the December issue of The Journal of Nuclear Medicine. In the first long-term study of intraarterial peptide receptor radionuclide therapy (PRRT) in advanced meningioma, patients saw improved radiologic and clinical disease control compared with intravenous PRRT, with no additional toxicity.
Radionuclide therapy delivered directly to an artery is feasible and safe for patients with advanced meningioma, according to new research published in the December issue of The Journal of Nuclear Medicine. In the first long-term study of intraarterial peptide receptor radionuclide therapy (PRRT) in advanced meningioma, patients saw improved radiologic and clinical disease control compared with intravenous PRRT, with no additional toxicity.
Meningiomas are the most common primary neoplasms of the central nervous system and account for more than one-third of all cases. Meningiomas are mostly classified as benign, but 10–15 percent of cases are considered atypical or malignant. The preferred treatment is surgery with external beam radiotherapy. However, 30–40 percent of lesions are ineligible for surgery due to their location. Furthermore, recurrence rates are notably high.
“For meningioma patients who are ineligible for surgery or who experience tumor recurrence, treatment options are limited,” stated Adriana Amerein, MD, nuclear medicine resident at University Hospital Augsburg in Augsburg, Germany. “Due to the high expression of somatostatin receptors in most meningiomas, radiopharmaceutical therapy offers a viable therapeutic alternative for patients. Intraarterial administration of the radiopharmaceutical might boost the achievable radiation dose to the tumor.”
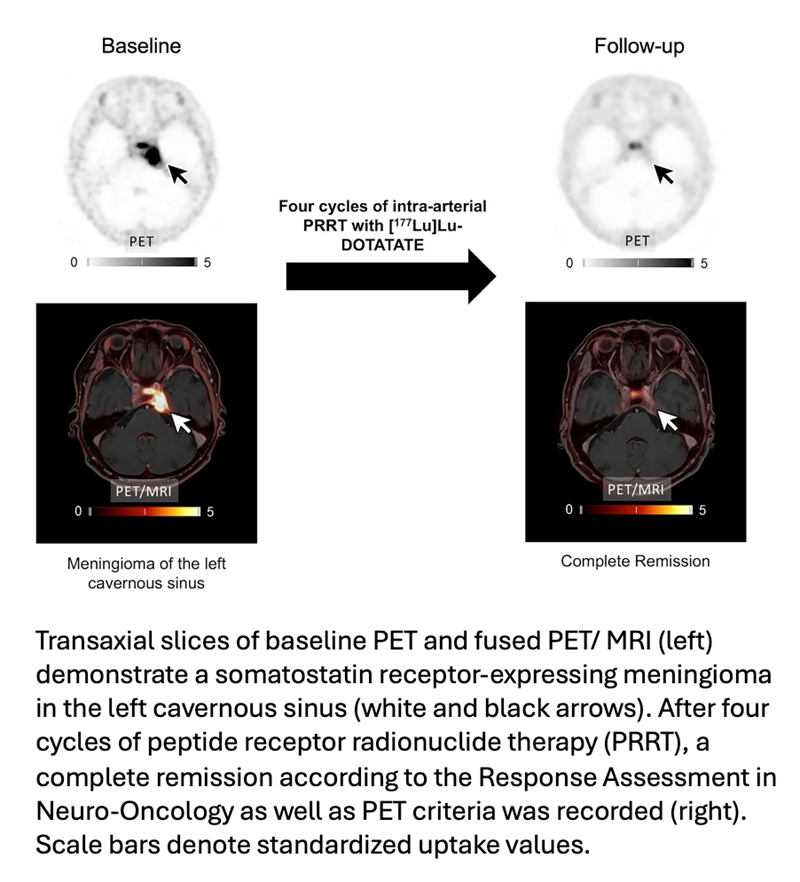
In the study, researchers assessed the long-term safety and efficacy of intraarterial PRRT in patients with advanced, progressive meningioma. Thirteen patients underwent one to four cycles of intraarterial PRRT with177Lu-HA-DOTATATE. Safety and treatment response was evaluated according to medical criteria, and results were compared with intravenous PRRT.
Treatment with intraarterial PRRT was well tolerated, with only transient adverse effects. The median progression-free survival for intraarterial PRRT was 18 months, and the median overall survival was not reached after 43 months. Approximately 80 percent of the patients showed radiologic disease control after intraarterial PRRT, compared to 40 percent after intravenous PRRT.
“These findings show that intraarterial administration of radiopharmaceutical therapy in meningioma is feasible, safe, and could be a promising therapeutic option in the future,” said Constantin Lapa, MD, nuclear medicine physician at University Hospital Augsburg. “Looking forward, personalized dosing and combination therapies utilizing intraarterial PRRT could further improve results for patients who don’t respond to conventional therapies.”
